Every so often, a medicine catches attention not just because it works, but because people keep asking if it’s as good as some say—or as risky. That’s exactly what happens with Arcoxia. Popped for back pain? Doctors recommend it for arthritis? Even pro athletes know the name. Everyone seems to have a friend or an aunt who swears by it, but there are just as many who warn, “Don’t mess with it.”
Arcoxia is one of those prescription pills you hear about in pain relief conversations. Some consider it their last savior for stubborn pain, while others nearly gasp at the idea of taking it for more than a few days. What’s the real deal here? You’re about to find out everything worth knowing—no jargon, no hype, just the facts and real talk.
What Exactly Is Arcoxia?
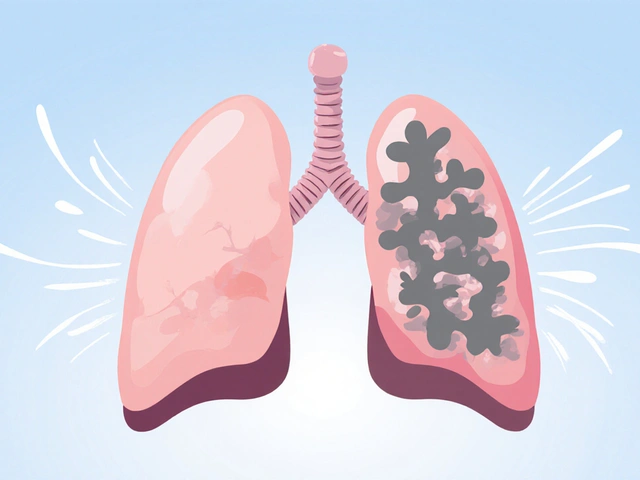
Arcoxia isn’t just a fancy name—it’s the brand name for etoricoxib, a nonsteroidal anti-inflammatory drug (NSAID). Unlike the standard ibuprofen you pick up at the grocery store, Arcoxia is a bit fancier. It focuses on one type of enzyme, COX-2, that’s a big driver of inflammation and pain in the body. Other NSAIDs, like naproxen or diclofenac, block both COX-1 and COX-2. Blocking just COX-2 aims to lower side effects on your stomach and gut lining. That’s the main pitch that’s fascinated doctors and patients since it hit pharmacies in the early 2000s.
Now, here’s an interesting bit—Arcoxia isn’t available everywhere. You’ll find it in most of Europe, parts of Asia, Australia, and South America. But in the United States, the FDA has repeatedly denied its application due to safety concerns around the heart. So, if you’re reading this in America, no, you weren’t just missing it on the pharmacy shelf.
Doctors reach for Arcoxia mainly for things like osteoarthritis, rheumatoid arthritis, ankylosing spondylitis, and gout attacks. Some post-surgery patients get it too, because it can tackle moderate pain and swelling without the tummy drama old-school NSAIDs can whip up. Sometimes, people with sensitive stomachs or ulcers who need pain relief long-term are prescribed Arcoxia.
When it comes to dosage, your doctor will set the lowest amount that actually works for you. Doses usually range from 30 mg to 120 mg daily, depending on what’s being treated. Gout attacks get the big guns at 120 mg for a short burst; chronic conditions like arthritis get a softer touch. Usually, one dose per day does the trick—no popping pills every few hours.
Arcoxia comes as tablets. Swallow it with water, same time every day, with or without food. Some people say it’s easier on an empty stomach, but others prefer it after breakfast to ward off queasiness. You’ll see effects within the first day or two—pain and swelling start backing down. For arthritis? It might take a week before it really feels like it’s helping, so patience matters.
Is Arcoxia addictive? Not even close—it’s not an opioid and doesn’t mess with your brain’s reward system. Stop it, and withdrawal isn’t a thing. But don’t just quit without telling your doctor if you’re on a long-term plan, because your pain or inflammation could bounce back hard.

How Well Does Arcoxia Work and Who Actually Needs It?
So what can Arcoxia actually do for you? It turns out, quite a lot, if you’re the right candidate. In head-to-head studies against regular NSAIDs like diclofenac or naproxen, Arcoxia stands up pretty well for pain relief and reducing inflammation—sometimes even outperforms them, especially for arthritis symptoms. People with osteoarthritis, that annoying wear-and-tear joint pain, often report less stiffness and swelling within days of starting it.
Rheumatoid arthritis is a nastier disease, eating away at joints with chronic inflammation. Here too, long-term patients often find everyday life a bit more doable with Arcoxia on board. Same with ankylosing spondylitis—a back disease that can almost lock up your spine. One study in Europe tracked patients for six months and saw meaningful improvements in pain scores compared to folks on placebo or standard NSAIDs.
The real buzz, though, is for those who can’t stomach regular NSAIDs. Stomach ulcers, heartburn, or bleeding? That’s where Arcoxia’s claim shines—it’s less likely to cause major stomach upsets because it leaves COX-1 alone. Still, “less likely” doesn’t mean zero risk. Some people still get heartburn, so you shouldn’t drop other stomach medications (like a PPI) without talking to your doctor.
Got a sudden, brutal attack of gout in your big toe? Arcoxia is on the menu for short, sharp pain. Another fun fact—rugby players and Olympic athletes have taken it (with medical supervision, of course) after joint injuries or tough matches, because it helps with swelling and can get them back to training quicker. It’s not a magic fix, but when rest isn’t an option and over-the-counter painkillers do nothing, Arcoxia sometimes steps up.
But here’s the kicker: Not everyone should—or can—take Arcoxia. If you’ve ever had a bad reaction to other NSAIDs, you need to tell your doctor everything. People with severe liver or kidney disease usually get ruled out. And if you’ve ever had heart problems, strokes, or even high blood pressure that won’t quit, Arcoxia gets risky in a hurry. There’s a reason why some heart specialists groan when they see it on a patient’s chart.
Dosing is all about your personal health. If you’re thin and healthy, the standard dose might work. If you’re older, have heart or kidney issues, or take other meds (like blood thinners or anti-hypertensives), your doc will go slow and steady, monitoring for any sneaky side effects. You might even get blood tests every few months to check your liver and kidney function. Overdosing doesn’t happen often, but if you ever take too much, you need medical help right away—there’s no quick fix at home.
Now, what about mixing Arcoxia with other drugs? Some interactions can be serious. If you’re already taking diuretics, certain antidepressants, or drugs to prevent blood clots, your pharmacist needs to know. Two medicines can either boost or cancel each other out—or worse, make side effects worse. Even simple stuff like herbal supplements or the grapefruit sitting in your fridge can factor in. Always mention every pill and over-the-counter thing you use—that’s not a suggestion, it’s survival smarts.

Side Effects, Risks, and Safe Use of Arcoxia
This is where things get real. You probably heard a thing or two about Arcoxia’s risks or scary side effects, especially heart attacks and strokes. Here’s what’s known—Arcoxia, like the rest of the COX-2 drug family, was created to dodge the gut issues of older NSAIDs. But it left the door open for more trouble with your heart and blood vessels. In fact, its close cousin, Vioxx (rofecoxib), got yanked off U.S. shelves years ago for exactly that reason. That’s why the FDA still says “no thanks” to Arcoxia, even though Europe, Asia, and Australia let it be prescribed with heavy warnings and guidelines.
The most common side effects? Some folks get headaches, dizziness, swelling of the legs or face, or flu-like feelings. Fluid retention is weirdly common with Arcoxia. If your socks leave major marks on your ankles or your ring gets tighter than usual, you should let your doctor know. It doesn’t mean a heart attack is coming—but it could be a sign you’re holding on to too much water.
Stomach problems—technically less frequent than regular NSAIDs, but not impossible. You still can get nausea, tummy pain, heartburn, or, rarely, ulcers and GI bleeds. The older you are, or the longer you take it, the more risk you take on. Kidneys also deserve a mention—a healthy person might see a small, reversible bump in kidney markers, but if you’ve got kidney issues already, Arcoxia can push you into dangerous territory.
The scary stuff mostly targets your heart. If you have a history of heart attack, stroke, angina, or uncontrolled high blood pressure, think twice. There’s agreement between cardiologists and rheumatologists: Long-term use of Arcoxia (at high doses) slightly raises your risk of cardiovascular problems, especially in folks who already have risk factors. That’s why every leaflet, every packaging, and every honest doctor will underline this before you get started.
Here’s a checklist you can run through before starting Arcoxia:
- Talk to your doctor about your full medical history—especially any history of ulcers, heart disease, liver disease, kidney problems, or allergies to NSAIDs.
- List every single medication you’re on, including vitamins, herbal supplements, and over-the-counter products.
- Follow the prescribed dose. Never double up or take more than the recommended daily amount.
- Watch for new symptoms—unusual swelling, shortness of breath, chest pain, yellowing of the skin or eyes (which could signal liver issues), or black/tarry stools (a sign of GI bleeding).
- Attend follow-up appointments. Blood pressure checks and blood tests aren’t just busywork—they keep you safe from silent side effects.
- If you’re trying to get pregnant, are already pregnant, or breastfeeding, stay away from Arcoxia unless your doctor finds no better option. It’s not considered safe here.
- Alcohol and Arcoxia don’t mix well. Booze increases the risk of stomach issues. Go easy or avoid drinking altogether when on this med.
- Keep Arcoxia out of reach of kids. Accidental overdoses have happened, especially with curious toddlers or pets.
When it comes to pain relief medicines, everyone wants a magic bullet—but there isn’t one. Arcoxia works well for muscle, bone, and joint pain when used right and for the right people. It’s not about “good” or “bad.” It’s about fit. Some swear by it, some can’t tolerate it at all. If you want to ask your doctor about Arcoxia, arm yourself with questions—know your risks, your other options, and what counts as an emergency side effect. And don’t be shy about seeking a second opinion if you’re on this drug long-term.
The bottom line with Arcoxia (or any powerful medicine): Know why you’re taking it, stick to your doctor’s plan, and never ignore weird symptoms. Pain can be stubborn, but health is always more stubborn. When you find a balance with the right pain relief and the least trouble, you win. That’s the real secret with *Arcoxia* and every pill like it.





Dan Burbank
July 18, 2025 AT 13:14Honestly, digging into Arcoxia, it's quite the subject. It's one of those NSAID class drugs that supposedly knocks down inflammation and pain, but really, the way it's marketed feels almost theatrical, doesn't it? People seem to jump on it expecting a miracle cure for arthritis or gout, but the side effects—often glossed over—can be quite serious, especially cardiovascular risks. So, before you buy into the hype, consider how mainstream medicine sometimes turns these pills into quick fixes without diving deep into long-term harm.
And let's not even start on how doctors sometimes prescribe it liberally without fully discussing alternatives. If you ask me, understanding the drug’s mechanism, mainly COX-2 inhibition, is crucial, but it's equally important to weigh the benefits and adverse effects critically. I mean, some patients do get relief, but at what price? The drama surrounding its safety profile is something every potential user should digest thoroughly.
Anna Marie
July 19, 2025 AT 17:46Thanks for sharing this post. I really appreciate the clarity it provides on Arcoxia's uses and risks. From what I understand, it’s important for patients to have access to detailed yet easy-to-understand explanations about their medications.
In my experience, empathy goes a long way when discussing treatment options with patients who might be worried about side effects. It’s about balancing effectiveness with safety. For example, if someone suffers chronic joint pain, knowing why Arcoxia is prescribed and the real nature of its benefits can be reassuring.
It would be helpful if the post also included advice on communicating with healthcare providers about dosage and monitoring. That way, users feel empowered, not just informed.
Abdulraheem yahya
July 21, 2025 AT 05:29Interesting stuff! I just wanna point out that in many parts of the world, access to drugs like Arcoxia is a blessing because alternatives can be scarce or unaffordable. People dealing with ongoing inflammatory conditions might not have the luxury to be too picky.
That said, the side effects are no joke, and they need to be looked at closely. But I feel the discussion often misses the socio-economic angle here. When you have a drug that offers relief, even if with risks, what do you do if nothing else comes close?
Also, I think there's a huge need for more public awareness campaigns that educate potential users on how to use such meds responsibly, not just the doctors and pharma companies.
Preeti Sharma
July 22, 2025 AT 05:13Isn’t it fascinating how we often view these medications as godsend potions without pondering the deeper implications? Arcoxia, for instance, is clearly another cog in the pharmaceutical machine—selling relief but also subtly normalizing dependency on chemical interventions.
Moreover, the very notion of ‘side effects’ seems oddly sanitized, as if they are mere footnotes rather than integral parts of the drug’s identity. Does the patient consent truly encompass understanding these risks psychologically and existentially, or is it just a legal formality?
Question: How do we reconcile our desperate desire for pain relief with the philosophical cost of masking bodily signals that are fundamentally part of our human experience?
Ted G
July 24, 2025 AT 13:36Watch out with Arcoxia, folks. I can't help but feel there's more behind these drugs than we are told. Big pharma pushing these pills knowing full well about the risks but keeping the info under wraps. A classic hustle. You take it for pain relief today and maybe get heart issues down the line—convenient, isn't it?
Plus, the whole process of drug approval is murky as hell. How many people have suffered quietly? I wouldn't be surprised if this drug's popularity is partly because it lines pockets rather than truly improves health.
Anybody else suspect the mainstream isn't telling the whole story about safety and long-term effects? Always question.
Miriam Bresticker
July 26, 2025 AT 05:20Heyyy I saw this and just had to comment! 🌟 So Arcoxia is like this cool magic thing but you gotta be super careful right? ✨ It’s all about balancing good and bad vibes aka relieving your discomfort without those pesky side effects messing up your day.
I’ve read about people feeling amazing with it and others not so much huh? Soooo it's def crucial to chat with your doc and keep an eye on how you feel. 🧐👩⚕️
Anyways, thanks for posting such an easy-to-get rundown on it, helps loads! 🌈💊
Claire Willett
July 28, 2025 AT 08:26Arcoxia serves as a selective COX-2 inhibitor, reducing prostaglandin production and thus mitigating pain and inflammation. Its pharmacokinetics allow for once-daily dosing, which enhances patient compliance.
However, clinicians must vigilantly observe cardiovascular profiles before prescribing, considering the elevated thrombotic risk associated with this class of drugs.
When managing patients with osteoarthritis or rheumatoid arthritis, the drug's efficacy is notable, but balancing risk-benefit ratios is paramount to optimizing therapeutic outcomes.
Keli Richards
July 30, 2025 AT 20:26I've taken Arcoxia for a few months, prescribed by my rheumatologist, and honestly, it helped reduce the joint pain that kept me up at night. The post is a fair summary, but I’d add that monitoring liver and kidney function is something doctors stress a lot with this med.
Side effects can vary, but for me, mild stomach discomfort was the biggest issue. Nothing unbearable, though. I was warned about cardiovascular risk and told to avoid it if I had hypertension.
Anyone else here using it long term? Curious how it's working out for others in different countries.
Ravikumar Padala
August 2, 2025 AT 17:53Ugh, I am always skeptical about drugs like Arcoxia. It’s another overhyped miracle pill if you ask me, and the side effects seem glossed over in most articles. A simple overview doesn’t cut it for those of us who worry about every detail.
I wish the discussion was more comprehensive about interactions with other meds and the impact on chronic diseases. People seem too quick to accept such drugs without demanding extensive research transparency.
King Shayne I
August 12, 2025 AT 14:00Medical industries designed this drug to be peddled everywhere yet it's a ticking time bomb for heart attack risks. It’s no coincidence they push it for arthritis or pain; those are very profitable markets. Don’t let anyone convince you differently.
You gotta scrutinize every pill offered. This isn’t just about medicine, it’s about profit-driven motives disguised as healthcare.
Anyone else here read the studies showing increased cardiovascular events? Wake up.
jennifer jackson
August 17, 2025 AT 13:14I've had arthritis for years, and coming across this post was reassuring. Sometimes it’s hard to believe in a medicine after so many disappointments, but understanding what Arcoxia does helps me stay hopeful.
Sure, side effects exist, but I believe with proper care, the benefits can outweigh the risks. It's about optimism and being proactive—listening to your body and communicating with your doctor regularly.
Thanks for spreading reasonable info! It's needed.