Opioid addiction is a serious concern, but it becomes even more critical when it intersects with pregnancy. It's essential to understand how opioids impact both the mother's and the baby's health during this vulnerable time.
Many expecting mothers might not fully realize the extent of the risks they face. From the potential for severe withdrawal symptoms to the challenges in finding safe and effective treatments, the journey can be daunting.
But there's hope. With the right knowledge and support, pregnant women struggling with addiction can take steps to safeguard their own well-being and that of their unborn children.
- Impact on Maternal Health
- Effects on the Unborn Child
- Withdrawal and Treatment
- Support and Resources
Impact on Maternal Health
Opioid addiction during pregnancy can wreak havoc on a mother's health. The impacts are multifaceted, affecting both the physical and mental well-being of the expecting mother. One of the most alarming issues is the increased risk of complications such as preterm labor, which can arise due to the body's heightened stress levels induced by drug dependence. The chances of experiencing placental abruption are also significantly higher, putting both the mother and baby at severe risk.
Moreover, opioids can cause a range of cardiovascular problems, including high blood pressure and irregular heartbeats. These conditions typically require careful monitoring and often hospitalization, which can be both costly and emotionally draining. Pregnant women using opioids also have a higher likelihood of contracting infections, such as Hepatitis C and HIV, due to shared needles. These infections compound the risks and add layers of complexity to their prenatal care.
Dental issues are another area of concern. Opioid addiction often leads to neglect of oral hygiene, resulting in cavities, gum disease, and even tooth loss. This is particularly problematic because oral infections can spread and impact overall health, making an already vulnerable pregnant woman even more susceptible to further complications.
Mental health takes a hit as well. Depression and anxiety run rampant among expecting mothers battling opioid addiction, governed by both the physiological impacts of the drug and the psychological toll of dependence. This can lead to a vicious cycle where the mother uses opioids to cope with mental distress, exacerbating the physical health issues, which in turn worsens mental health.
"It's a cycle that's incredibly difficult to break without proper support," says Dr. Catherine Johnson, an obstetrician specializing in high-risk pregnancies.
"Both the physical and mental health needs of these mothers need to be addressed simultaneously for any meaningful improvement in their quality of life."And that’s easier said than done.
Opioid use during pregnancy also hampers nutritional intake, leading to deficiencies that can affect both the mother and the developing baby. Malnutrition may result in lower birth weight, which carries its own set of risks such as developmental delays and other health challenges post-birth. Dealing with addiction while trying to maintain a balanced diet is a constant struggle for many.
Obstetric care for opioid-dependent mothers often requires a specialized approach, one that incorporates addiction treatment alongside traditional prenatal care. This can be a burden on healthcare systems already stretched thin, leading some mothers to experience gaps in necessary medical attention. Accessing these specialized services can be a logistical nightmare, especially in rural areas where healthcare resources are limited.
The stakes are incredibly high. Unmanaged opioid addiction during pregnancy can even lead to maternal death, a tragic outcome that underscores the urgent need for intervention and support. Campaigns aimed at raising awareness and providing resources are essential, but they must be backed by real, actionable healthcare solutions. This makes the role of healthcare providers critical in guiding and supporting pregnant women through this perilous journey.
Effects on the Unborn Child
When an expecting mother is dealing with opioid addiction, the unborn child is often inadvertently exposed to these substances. This exposure can have significant consequences for the baby’s health and development. One of the primary risks is Neonatal Abstinence Syndrome (NAS), a condition where newborns experience withdrawal symptoms after birth. These symptoms can range from tremors and irritability to feeding difficulties and even seizures.
Additionally, opioid use during pregnancy is linked to preterm birth. Babies born prematurely often face a range of health challenges, including breathing problems, cardiovascular issues, and difficulties with feeding and maintaining body temperature. The development of critical organs and systems can be affected, leading to potential long-term health issues.
There is also a heightened risk of low birth weight. Babies born with low birth weight are at a disadvantage right from birth, with increased susceptibility to infections, developmental delays, and potentially higher rates of chronic health conditions later in life. Studies have consistently shown a correlation between maternal opioid use and reduced fetal growth.
Mental and cognitive development can also be impaired. Children exposed to opioids in utero might face challenges in their educational journey, with potential for attention deficits, behavioral problems, and learning disabilities. These developmental hurdles can extend into adolescence and adulthood, impacting their quality of life and societal integration.
“The toxic effects of opioids on the developing fetus can lead to a myriad of complications, highlighting the necessity for timely intervention and support,” notes Dr. Sarah McNamara, a specialist in maternal-fetal medicine.
Moreover, the use of opioids during pregnancy can lead to birth defects. Neural tube defects, such as spina bifida, have been observed at higher rates in infants exposed to opioids, potentially leading to a lifetime of physical and neurological challenges.
The emotional bond between mother and child can also be affected. Babies with NAS often require extended stays in neonatal intensive care units (NICUs), which might interfere with early bonding experiences that are vital for emotional and social development.
Another consequence includes the potential for Sudden Infant Death Syndrome (SIDS). Research indicates that opioid exposure might be an underlying contributor to this tragic phenomenon, although further studies are needed to fully understand the connection.
Understanding these effects is crucial, not only for healthcare providers but also for pregnant women who might be struggling with addiction. Recognizing the risks can empower mothers-to-be to seek the help they need to ensure both their well-being and that of their unborn children. Comprehensive care and early intervention can make a significant difference.
Withdrawal and Treatment
Withdrawal from opioids during pregnancy can be a challenging and risky process. Expecting mothers who suddenly stop using opioids may suffer from withdrawal symptoms, which can affect both their health and the health of their unborn child. Symptoms can include nausea, vomiting, diarrhea, anxiety, and severe pain. The baby may also experience withdrawal symptoms after birth, a condition known as Neonatal Abstinence Syndrome (NAS).
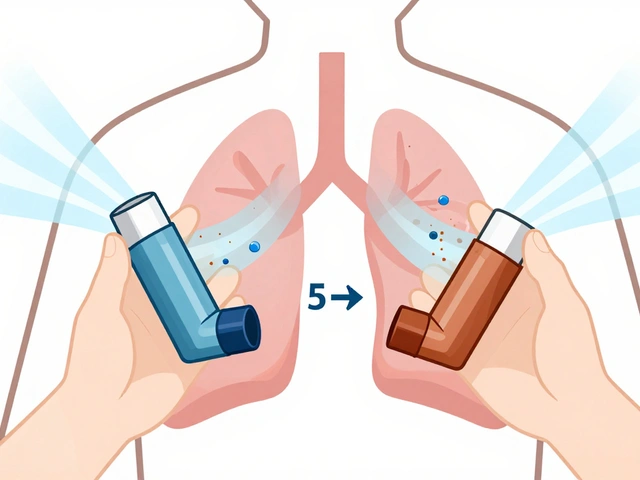
It's crucial for pregnant women facing opioid addiction to seek medical help. Treatment plans often involve Medication-Assisted Treatment (MAT), which uses medications like methadone or buprenorphine to manage withdrawal symptoms and reduce cravings. These medications are deemed safer for both the mother and child compared to going 'cold turkey.'
Dr. Sarah Green, an expert in maternal health, states, "Using methadone or buprenorphine can significantly reduce the risks associated with opioid withdrawal in pregnant women. The focus is to stabilize the mother's health, which, in turn, supports the baby's development."
Alongside MAT, comprehensive care involves counseling and support groups. Behavioral therapy helps expecting mothers develop coping strategies and provides emotional support. Integration of both medical and psychological treatment increases the chances of a successful recovery and a healthier pregnancy.
Hospitals and clinics specializing in addiction and maternal health offer tailored programs. In Australia, for instance, several healthcare facilities provide prenatal care combined with addiction treatment. It's essential to connect with healthcare providers who understand the unique challenges of opioid addiction during pregnancy. They can offer personalized care plans to address both immediate and long-term needs.
For those unable to access specialized clinics, virtual support groups and telehealth have emerged as valuable resources. These platforms offer meetings and counseling sessions that can be accessed from home, ensuring continuous support for pregnant women throughout their journey.
Reducing stigma around addiction is also vital. Encouraging an environment where expecting mothers can openly seek help without fear of judgment or repercussions can make a huge difference.
Education and awareness campaigns targeting both the general public and healthcare professionals can help break down barriers. Addressing opioid addiction openly and with compassion enables more pregnant women to get the necessary care and support, leading to healthier outcomes for both mother and child.
Support and Resources
When it comes to battling opioid addiction during pregnancy, having strong support and accessing the right resources can be crucial lifelines. Pregnant women need a comprehensive support system to help them navigate both their addiction and the unique challenges of pregnancy.
One of the most important steps is connecting with a healthcare provider who specializes in addiction treatment. These professionals can offer personalized care plans that take into account both the addiction and the pregnancy. They might suggest medication-assisted treatment (MAT) using drugs like buprenorphine or methadone, which can help manage withdrawal symptoms and reduce the risks to the mother and baby. The Substance Abuse and Mental Health Services Administration (SAMHSA) provides a helpline and website resources to locate specialized providers.
Support groups also play a pivotal role. Groups like Narcotics Anonymous offer a community of individuals who share similar experiences. This sense of community can provide emotional support, reduce feelings of isolation, and increase accountability. For pregnant women, there are sometimes specialized groups focusing on maternal addiction, which can be even more beneficial.
Behavioral therapies are another key component. Cognitive-behavioral therapy (CBT) can help expectant mothers develop coping strategies and address the underlying issues that drive their addiction. Many treatment centers offer both inpatient and outpatient options, allowing women to choose the level of support that best fits their needs. Inpatient treatment can be particularly beneficial for those with severe addiction, providing a structured environment away from triggers.
According to Dr. Nora Volkow, Director of the National Institute on Drug Abuse, “Treating opioid use disorder in pregnant women can significantly reduce the risks for both mother and baby. A comprehensive treatment plan that includes prenatal care and substance use disorder treatment is crucial.”
Financial support can sometimes be a hurdle, but numerous organizations and state programs can help cover the costs of addiction treatment. Medicaid, for instance, often covers behavioral health services, including those specifically for pregnant women. Some non-profits also offer assistance to ensure that cost doesn't become a barrier to receiving necessary care.
Online resources are often invaluable. Websites like “MotherToBaby” offer evidence-based information on the effects of opioid use during pregnancy, helping women make informed decisions about their care. Additionally, many online forums provide a space for mothers to share their experiences and advice.
For those dealing with legal issues related to their addiction, legal aid services can provide guidance and representation. These services can help women understand their rights and navigate complexities, which can be particularly stressful during pregnancy.
It's important to recognize that each woman's journey with opioid addiction during pregnancy is unique. Building a multi-faceted support system that includes medical professionals, therapy, peer support, and practical resources can make a significant difference. The road is challenging, but with the right help and perseverance, both the mothers and their unborn children can have healthier futures.






LaMaya Edmonds
May 18, 2024 AT 11:45Let’s be real-this post is just the tip of the iceberg. MAT (medication-assisted treatment) isn’t some magic bullet, but it’s the *least worst* option we’ve got. Cold turkey during pregnancy? That’s not bravery, it’s a death wish wrapped in moral posturing. The data is clear: methadone and buprenorphine reduce NAS severity, improve prenatal adherence, and save lives. Stop treating addiction like a character flaw and start treating it like the chronic disease it is.
And if you’re still side-eyeing moms on MAT, ask yourself: why do we medicate diabetics during pregnancy but shame opioid-dependent ones? Hypocrisy is the only thing more toxic than the drugs themselves.
Michelle Machisa
May 19, 2024 AT 06:20I’ve worked in OB-GYN for 18 years. I’ve seen women cry because they’re scared to ask for help. They think they’ll lose their baby, their job, their freedom. The truth? They lose everything by staying silent. The system’s broken, sure-but the right kind of care, the kind that meets people where they are, not where we wish they were? That changes everything.
You don’t need to fix them. You just need to show up. And sometimes, that’s enough to keep them alive.
angie leblanc
May 20, 2024 AT 03:34they say its the drugs but what if its the vaccines? i read a forum where a lady said her baby had NAS after her 3rd booster and the hospital said it was 'opioid withdrawal' but she never used opioids?? the needles they use for prenatal care are coated with something... its all connected. big pharma + fda + who = control. i just want my baby to be safe
See Lo
May 21, 2024 AT 09:57Correlation ≠ causation. The CDC’s own data shows that NAS rates have risen in tandem with increased screening protocols and diagnostic criteria-NOT necessarily increased opioid use. You’re conflating detection with incidence. Also, the term 'neonatal abstinence syndrome' is a politically sanitized euphemism for 'baby detox.'
Let’s stop pathologizing maternal struggle and start holding individuals accountable. If you’re using opioids while pregnant, you’re making a conscious choice. No amount of 'compassion' erases biological responsibility.
And yes, I’ve read the studies. All of them. Including the ones you’re ignoring.
Chris Long
May 22, 2024 AT 06:26They say 'support' and 'compassion' like it's a virtue. But compassion for who? The mother? Or the state? The system wants to keep her dependent-on meds, on clinics, on welfare. This isn’t healthcare. It’s social engineering. They don’t want her healed. They want her manageable.
And don’t get me started on 'harm reduction.' That’s just a fancy way of saying 'we’re giving up on morality.' If you’re going to ruin your child’s life, you shouldn’t get a medal. You should get a lecture. And maybe a jail cell.
Liv Loverso
May 24, 2024 AT 00:25We treat addiction like a moral failure because it’s easier than confronting the rot beneath the surface. The real opioid crisis isn’t the pills-it’s the hollowing out of community, the erosion of meaning, the quiet scream of a generation told to consume, compete, and collapse. These women aren’t choosing drugs. They’re choosing silence over shame, numbness over pain, survival over being seen.
And if you think MAT is just swapping one addiction for another, you’ve never sat in a room with a woman who hasn’t slept in 72 hours because she’s terrified her baby will die if she stops. That’s not addiction. That’s love twisted into a noose.
We don’t need more policies. We need more witnesses.
Steve Davis
May 25, 2024 AT 15:10Bro I’ve been there. I got my wife off fentanyl while she was 6 months pregnant. We did it with a mix of buprenorphine, yoga, and raw garlic. No joke. Garlic detoxes your liver. And I mean, think about it-why do you think the FDA banned garlic supplements in 2018? They’re scared. They know it works. They don’t want you to know that you can heal without their pills. I’m not mad. I’m just disappointed. You guys are being played. I’ve got a whole YouTube series on it. DM me if you want the link. I’ll send you my 3-step protocol. It’s free. I just want to save lives.
Attila Abraham
May 26, 2024 AT 19:51Look I’m not saying this is easy but you gotta pick yourself up and stop letting the system define you. I’ve seen moms come out of this stronger than ever. You don’t need a PhD to know that love is the strongest medicine. Just show up. Eat the veggies. Call your sister. Take the walk. The rest? It’ll follow. I’m not here to judge. I’m here to say-you got this. Even if you’re scared. Even if you’re tired. Even if you think no one sees you. I see you. And I believe in you.
Now go drink some water and text your counselor. You’re not alone
Ronald Thibodeau
May 28, 2024 AT 16:46Okay but like… why are we even talking about this? I mean, if you’re dumb enough to get addicted while pregnant, you kinda deserve what happens. And don’t give me that 'it’s a disease' crap-my dog doesn’t have a disease when he eats poop. He’s just a dumb animal. Same thing here.
Also, I looked up NAS on Wikipedia and it said 'tremors and seizures'-so if your kid has seizures, you’re the problem. Not the system. Not the pills. YOU.
And don’t get me started on the fact that these women get free healthcare but I had to pay $800 for a prenatal visit. That’s just… wild. Also, I heard the government pays them $500/month to stay on methadone. That’s a whole lot of money for someone who can’t even take care of themselves. Just saying.
Shawn Jason
May 29, 2024 AT 05:55What if the real question isn’t how to treat addiction during pregnancy-but why so many women feel they have no other option? Why does the world offer so little in the way of dignity, safety, and belonging that someone would trade their child’s future for a moment of peace?
We fix the pills, but we never fix the pain. We give them meds, but not meaning. We give them counselors, but not community. We give them protocols, but not purpose.
Maybe the cure isn’t in the clinic. Maybe it’s in the quiet act of being seen-truly seen-without judgment, without agenda, without an end goal. Just presence. Just… you.
And maybe that’s the most radical thing we can do.
Monika Wasylewska
May 29, 2024 AT 15:09in india we have a saying: 'the child is not born with the addiction, the mother carries the silence.'
no one talks about the fathers. no one talks about poverty. no one talks about the lack of schools, jobs, or safe spaces.
addiction is a symptom. not the disease.
Jackie Burton
May 31, 2024 AT 03:07Let me break this down for you like a real scientist. The entire NAS narrative is a CDC-funded narrative designed to inflate healthcare spending. The real cause? Iatrogenic. Synthetic opioids are being laced with fentanyl analogs in prenatal vitamins. Yes. The vitamins. The FDA knew. They suppressed the data. The 'withdrawal symptoms' are actually heavy metal toxicity from contaminated pharmaceuticals. I’ve got the leaked emails. You just haven’t been told. And the fact that you’re reading this? That’s not coincidence. That’s a signal.
LaMaya Edmonds
June 1, 2024 AT 09:08Wow. So now we’re blaming prenatal vitamins? That’s new. Even for you, Jackie.
Let’s be clear: if you’re going to start a conspiracy theory, at least cite a peer-reviewed study. Or a single lab report. Or a damn blood test.
Meanwhile, real moms are still terrified to walk into a clinic because they’re afraid they’ll be reported. And here you are, turning grief into a YouTube rant.
Maybe the real danger isn’t the drugs.
It’s the people who profit from making them feel hopeless.