Medication-Acid Reducer Interaction Checker
Check if your medications might be affected by acid-reducing drugs like omeprazole, famotidine, or antacids. These medications can significantly reduce absorption of many other drugs.
How This Works
Acid reducers change your stomach pH, which can reduce absorption of certain medications. This tool helps you check if your medications might be affected based on data from FDA warnings and clinical studies.
When you take a proton pump inhibitor like omeprazole or an H2 blocker like famotidine for heartburn, you’re not just changing your stomach’s acidity-you’re changing how your body absorbs other medications. This isn’t a rare side effect. It’s a well-documented, clinically significant issue that affects thousands of people every year. And most of them don’t even know it’s happening.
Why Your Stomach Acid Matters for Medicines
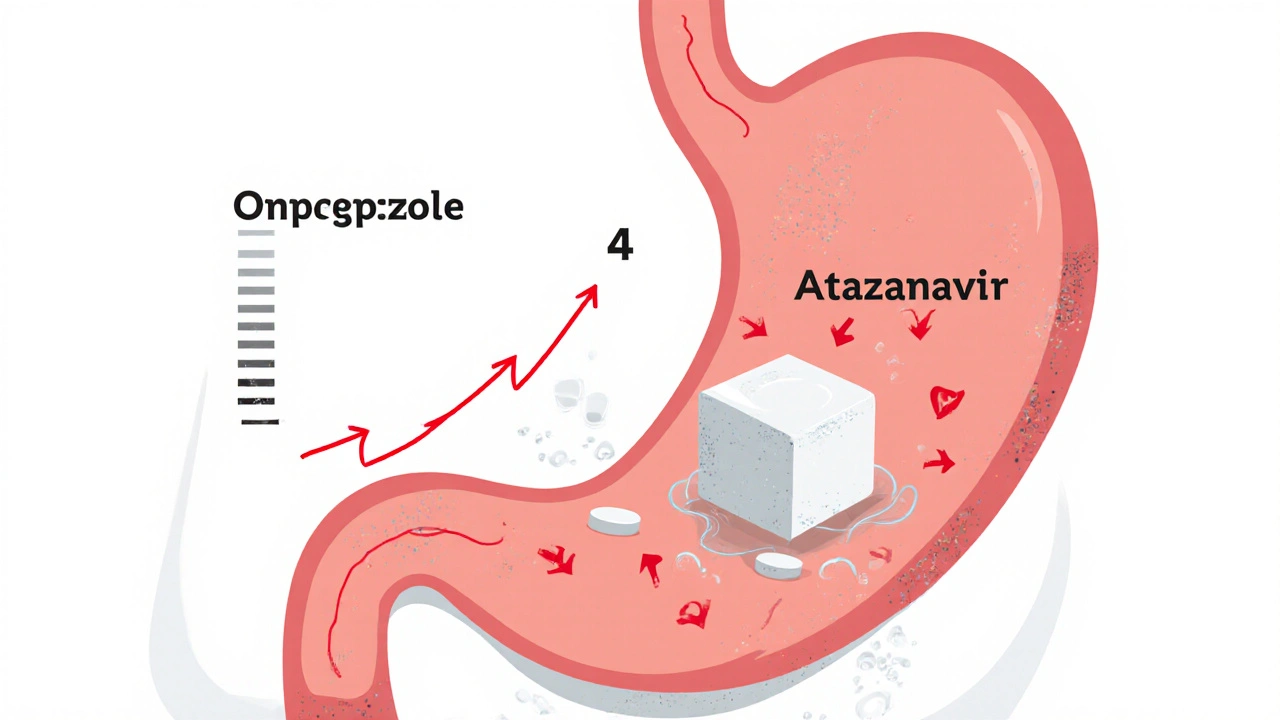
Your stomach is naturally acidic, with a pH between 1.0 and 3.5 when fasting. That acidity isn’t just there to digest food-it’s critical for breaking down and absorbing certain drugs. Many medications are weak bases, meaning they need an acidic environment to dissolve properly. When acid-reducing drugs like PPIs or H2 blockers raise your stomach pH to 4.0 or higher, these drugs stay in their non-ionized form, which makes them less soluble. Less solubility means less absorption. And if the drug doesn’t get into your bloodstream, it doesn’t work.Think of it like trying to dissolve sugar in cold water versus hot water. Sugar doesn’t dissolve well in cold water-it just sits there. Same thing with drugs like atazanavir or dasatinib in a high-pH stomach. They just don’t dissolve, and your body can’t absorb them.
The Top Drugs That Don’t Work With Acid Reducers
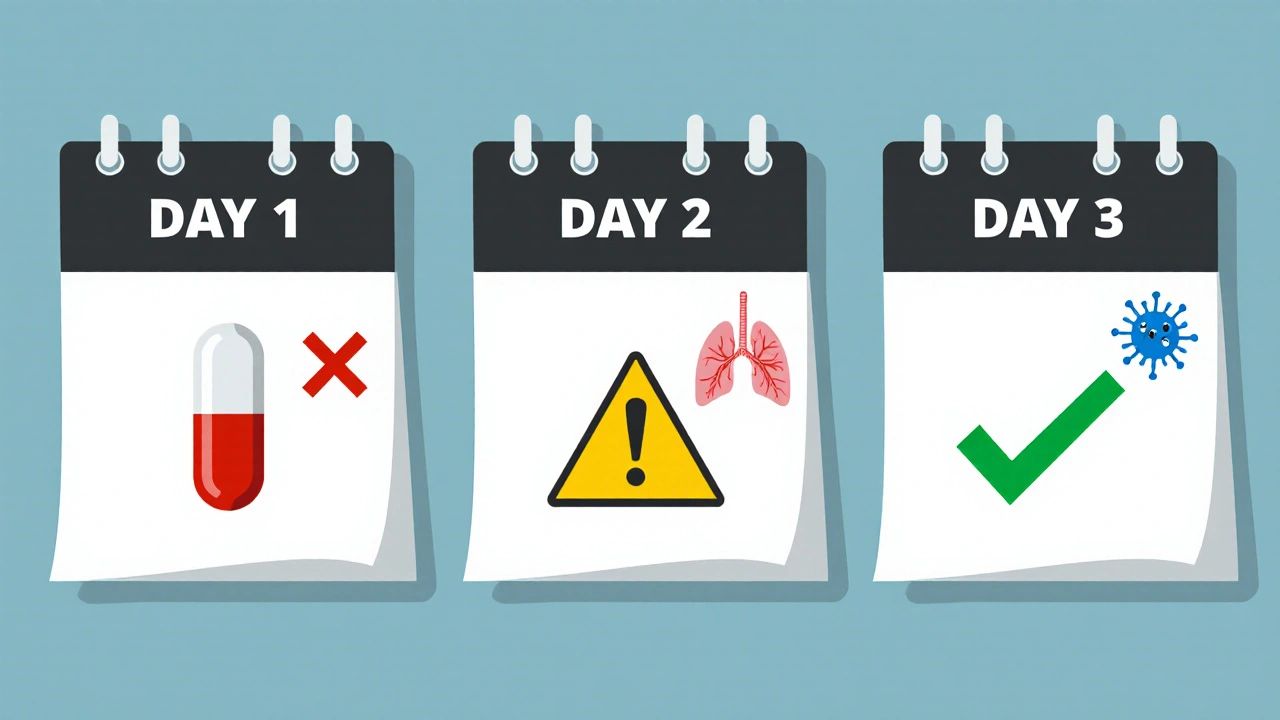
Some medications are especially vulnerable. The FDA has flagged 12 high-risk drugs with clear warnings. Here are the most common ones:- Atazanavir (HIV treatment): When taken with a PPI, absorption drops by 74% to 95%. This isn’t a small drop-it can cause viral rebound. Patients have reported their HIV viral load jumping from undetectable to over 12,000 copies/mL after starting omeprazole.
- Dasatinib (leukemia drug): Absorption falls by about 60%. A 2023 study of over 12,000 patients found those taking PPIs had 37% higher rates of treatment failure.
- Ketoconazole (antifungal): Absorption drops by 75%. At this level, the drug becomes practically useless.
- Nilotinib, erlotinib, mycophenolate: All show significant drops in absorption when paired with PPIs.
Even if you’re not on one of these, you might be on something else. About 25% to 50% of the top 200 prescribed drugs in the U.S. are weak bases that could be affected. That includes blood pressure meds, antidepressants, and even some antibiotics.
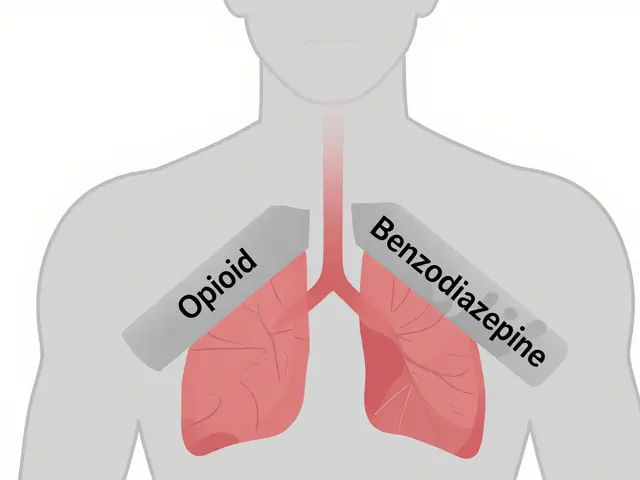
PPIs vs. H2 Blockers: Not All Acid Reducers Are Equal
Not all acid-reducing drugs are the same. PPIs (like omeprazole, esomeprazole, lansoprazole) are stronger and longer-lasting. They can keep your stomach pH above 4 for 14 to 18 hours a day. H2 blockers (like famotidine, ranitidine) only do it for 8 to 12 hours. That difference matters.A 2024 study in JAMA Network Open found PPIs reduce absorption of pH-dependent drugs by 40% to 80%. H2 blockers? Only 20% to 40%. So if you’re on a high-risk medication, switching from a PPI to an H2 blocker might help-but it won’t fix the problem entirely.
And timing doesn’t always save you. Some people think taking their medication two hours before the acid reducer will help. It does a little-maybe 30% to 40% better-but not enough for drugs like atazanavir. The FDA says even staggered dosing isn’t reliable for the highest-risk cases.

What About Antacids and Enteric Coatings?
Antacids like Tums or Maalox work fast but don’t last long. They can be used if you space them out-take your drug at least 2 to 4 hours before or after. But if you’re on a daily medication, that’s hard to stick with. Plus, antacids don’t prevent acid rebound, which can happen after they wear off.Enteric-coated pills are designed to dissolve in the intestine, not the stomach. Sounds safe, right? Not always. When stomach pH rises, these coatings can dissolve too early-right in the stomach-where they get destroyed by the remaining acid or cause irritation. The Merck Manual warns this can lead to reduced effectiveness or even stomach damage.
Real-World Consequences: When a Pill Stops Working
This isn’t theoretical. People are getting sick because their meds aren’t working.In one Reddit thread, a patient wrote: “My viral load went from undetectable to 12,000 after I started Prilosec for heartburn.” That’s not a fluke. The FDA’s adverse event database has over 1,200 reports of therapeutic failure linked to acid reducers between 2020 and 2023. Atazanavir, dasatinib, and ketoconazole top the list.
Another case: a woman on a blood pressure med noticed her readings were consistently 20 points higher. Her doctor didn’t think to check for interactions until she mentioned she’d started Nexium. Once they stopped the combination, her numbers returned to normal.
On the flip side, there’s good news. A 2022 study in the Journal of Clinical Oncology showed that when patients with leukemia took dasatinib 12 hours before their PPI, 85% regained full therapeutic response. Timing matters-but only if you know to do it.
Who’s Responsible for Catching This?
Doctors don’t always know. Pharmacists do.A 2023 study in the Journal of the American Pharmacists Association found that pharmacist-led medication reviews cut inappropriate acid reducer co-prescribing by 62% in Medicare patients. Pharmacists are trained to spot these interactions. They check every new prescription against every existing one. But if you’re filling prescriptions at different pharmacies, or if your doctor prescribes the acid reducer without telling your pharmacist, the system breaks.
Electronic health records now have alerts for high-risk combinations. Epic Systems reported that 78% of clinicians follow these alerts. But 22% still don’t. That’s 1 in 5 patients slipping through the cracks.
What You Can Do Right Now
If you’re on any of these drugs:- Check your list. Are you taking a PPI or H2 blocker? Omeprazole, pantoprazole, esomeprazole, famotidine, ranitidine?
- Look up your other meds. Search for “drug interaction” + your medication name. Use Drugs.com or Medscape. Look for warnings about “gastric pH,” “absorption,” or “PPI.”
- Ask your pharmacist. They’re the experts on this stuff. Don’t wait for your doctor to bring it up.
- Ask if you really need the acid reducer. The American College of Gastroenterology says 30% to 50% of long-term PPI users don’t have a valid reason. Deprescribing can eliminate the risk entirely.
- If you must take both, ask about timing. For weak bases, take the drug 2 hours before the acid reducer. But know that this isn’t foolproof.
The Bigger Picture: Why This Keeps Happening
The acid-reducing medication market is worth over $18 billion. PPIs are among the most prescribed drugs in the U.S. and Australia. But many people take them for years without reassessment. Heartburn isn’t always GERD. Sometimes it’s just diet or stress.The FDA has responded by requiring 28 new drug labels to include ARA interaction warnings since 2020-up from just 12 in the previous five years. The European Medicines Agency has done the same. But awareness still lags behind risk.
Pharmaceutical companies are starting to adapt. Nearly 40% of new drugs in development now use pH-independent delivery systems-like nanoparticles or enteric coatings designed to work regardless of stomach pH. That’s the future. But for now, the burden is on you and your care team to catch these interactions before they cause harm.
Final Thought: Your Meds Aren’t Just Sitting There
Medications aren’t magic pills. They’re chemicals that rely on your body’s chemistry to work. Changing your stomach’s pH isn’t a harmless tweak-it’s a major alteration to how your body handles drugs. What seems like a simple fix for heartburn could be quietly undermining your treatment for cancer, HIV, or heart disease.If you’re on more than one prescription, especially if one of them is for acid reflux, don’t assume everything’s fine. Ask the questions. Check the interactions. Talk to your pharmacist. You might be saving your life-not just your stomach.
Can I take antacids with my acid-reducing medication?
Yes, but timing matters. Antacids like Tums or Maalox work quickly but wear off fast. Take your other medication at least 2 to 4 hours before or after the antacid. Don’t use antacids as a long-term substitute for PPIs or H2 blockers-they’re not designed for daily, ongoing use.
Do all acid-reducing drugs affect medications the same way?
No. Proton pump inhibitors (PPIs) like omeprazole cause stronger and longer-lasting increases in stomach pH than H2 blockers like famotidine. PPIs reduce absorption of affected drugs by 40-80%, while H2 blockers typically reduce it by 20-40%. PPIs are also more likely to cause clinically significant interactions.
What should I do if my medication stops working after starting an acid reducer?
Don’t increase your dose. Contact your doctor or pharmacist immediately. Your medication may not be absorbing properly. They may need to switch your acid reducer, adjust your dose, change the timing, or find an alternative treatment that doesn’t interact. Never ignore a sudden change in how your medication works.
Are there any acid-reducing drugs that don’t interfere with other medications?
There’s no acid-reducing drug that’s completely free of interaction risk. But some medications, like sucralfate, don’t raise stomach pH and are less likely to interfere. However, sucralfate has its own limitations and isn’t used for long-term GERD. The safest approach is to avoid acid reducers unless they’re truly necessary-and to always check for interactions with your other meds.
Can I stop my acid reducer on my own?
No. Stopping PPIs or H2 blockers suddenly can cause rebound acid hypersecretion, making heartburn worse. Always talk to your doctor first. They can help you taper off safely, especially if you’ve been taking it for months or years. But if you’re on a high-risk medication, the benefit of stopping the acid reducer may outweigh the risk of rebound.





satya pradeep
November 17, 2025 AT 08:20Man i just found out my dad’s on omeprazole and atazanavir and he’s been feeling like crap for months. No one ever told him about this. I’m printing this out and taking it to his doctor tomorrow. This is wild how many people are just floating through life with meds that don’t work because no one connects the dots.
Kyle Swatt
November 17, 2025 AT 18:12Stomach acid isn’t just for digesting burritos-it’s the bouncer at the club of your bloodstream. Kick out the acid reducers and suddenly your cancer drug gets VIP access. Keep the acid in and your meds actually do their job. This isn’t science fiction. This is your body screaming for you to stop treating heartburn like a lifestyle choice.
Deb McLachlin
November 19, 2025 AT 10:45As a pharmacist, I see this every day. Patients come in with perfectly controlled hypertension, then start omeprazole for ‘a little indigestion’ and their BP spikes. We run interaction checks, but if the prescriber doesn’t document the reason for the PPI, we’re flying blind. This needs to be mandatory in EHR workflows-not just a pop-up alert that gets ignored.
Elia DOnald Maluleke
November 21, 2025 AT 03:01The human body is not a vending machine. Insert pill, receive cure. It is a symphony of chemistry, where a single note-altered pH-can silence an entire movement. To treat acid reflux as trivial is to misunderstand the architecture of life itself. We have forgotten that medicine is not an intervention, but a negotiation with nature. And nature, when insulted, does not whisper-it collapses.
Eric Healy
November 23, 2025 AT 02:04So what you’re saying is if I take my blood pressure med at 7am and my Tums at 11am I’m good? Lol no. The FDA says timing doesn’t work for high risk drugs and you’re acting like this is a scheduling problem. It’s a systemic failure. Doctors prescribe like they’re ordering coffee. ‘I’ll have the PPI with a side of dasatinib, no stir.’
saurabh lamba
November 23, 2025 AT 22:32So basically… acid reducers are the villain we all love to hate? 😅 I mean, I get it, but also… I just want to eat tacos without crying. Is there a middle ground? Or am I just doomed to be a walking drug interaction?
Bill Machi
November 24, 2025 AT 07:58Let me get this straight-you’re telling me some guy in a lab in 1988 invented a pill to stop heartburn, and now we’re sacrificing cancer patients and HIV patients because we got lazy? This isn’t medicine. This is corporate convenience dressed up as healthcare. We’ve turned the human body into a profit center and now we’re surprised when it breaks.
Kiran Mandavkar
November 25, 2025 AT 19:20Anyone who takes a PPI for more than 3 months without a gastroenterologist’s signature is not a patient-they’re a walking liability. And if your doctor didn’t warn you about this, they’re not a doctor, they’re a prescription machine. This isn’t ignorance-it’s malpractice by omission. Wake up.
Gordon Mcdonough
November 27, 2025 AT 10:11My wife took Prilosec for 4 years for ‘stress heartburn’… turned out she had a silent arrhythmia. The PPI masked the symptoms. We almost lost her. Don’t treat symptoms. Treat causes. And if you’re on more than one med, stop assuming everything’s fine. Ask. Always ask. Even if it feels dumb. Because dumb questions save lives.