When you’re struggling to breathe, the right inhaler can mean the difference between panic and relief. But if you don’t know bronchodilators from corticosteroids, you might be using them wrong-and missing out on real control over your breathing. These two types of medications don’t just treat symptoms; they work together to fix what’s broken inside your airways. And most people have no idea how or why.
What Bronchodilators Do (And When to Use Them)
Bronchodilators are your quick-fix inhalers. They’re the blue or gray ones most people reach for when they feel tightness, wheezing, or shortness of breath. These drugs don’t cure anything. They don’t reduce swelling. They simply relax the muscles wrapped around your airways, letting them open up so air can flow again.
There are two main types. Beta-2 agonists like albuterol (also called salbutamol) trigger a chemical signal in your lungs that tells the muscles to loosen. You feel the effect in 15 to 20 minutes, and it lasts 4 to 6 hours. That’s why they’re called short-acting bronchodilators (SABAs). They’re perfect for sudden flare-ups.
Then there are long-acting bronchodilators (LABAs) like salmeterol and formoterol. These take longer to kick in-around 30 minutes-but they keep working for 12 hours or more. They’re not meant for emergencies. Used alone, they can be dangerous. The SMART trial showed using LABAs without an anti-inflammatory drug increases the risk of asthma-related death by 3.5 times. That’s why they’re always paired with corticosteroids in combination inhalers like Advair or Symbicort.
Anticholinergics like ipratropium and tiotropium work differently. They block a nerve signal that makes airways tighten. Ipratropium works in 15 minutes and lasts 4 to 6 hours. Tiotropium lasts 24 hours, making it a go-to for COPD patients who need steady, all-day relief.
How Corticosteroids Actually Fix the Root Problem
While bronchodilators open the door, corticosteroids clean up the mess inside. These are the brown, orange, or white inhalers-often called “preventers” or “controllers.” They don’t give you instant relief. If you use one during an asthma attack, you’ll still be gasping. But if you take them every day, they slowly reduce the inflammation that makes your airways sensitive and swollen.
Inhaled corticosteroids like fluticasone, budesonide, and beclomethasone work at the genetic level. They enter lung cells and turn down over 100 genes that cause inflammation. They also turn on genes that help calm the immune system. This reduces mucus, swelling, and the constant “itch” in your airways that triggers coughing and wheezing.
The results? Regular use cuts asthma exacerbations by 30 to 60%, according to the American College of Allergy, Asthma & Immunology. It’s not magic-it’s biology. And it takes weeks. You won’t feel better right away. But after a month of daily use, you’ll notice fewer nighttime coughs, less need for your rescue inhaler, and fewer trips to the ER.
But there’s a catch. Corticosteroids can cause oral thrush-a fungal infection that makes your mouth feel sore and coated in white patches. About 5 to 10% of users get it. The fix? Rinse your mouth with water and spit after every use. No swallowing. No skipping. And if you’re on high doses-over 1,000 mcg of fluticasone daily-you’re at higher risk for pneumonia, especially if you’re over 65.
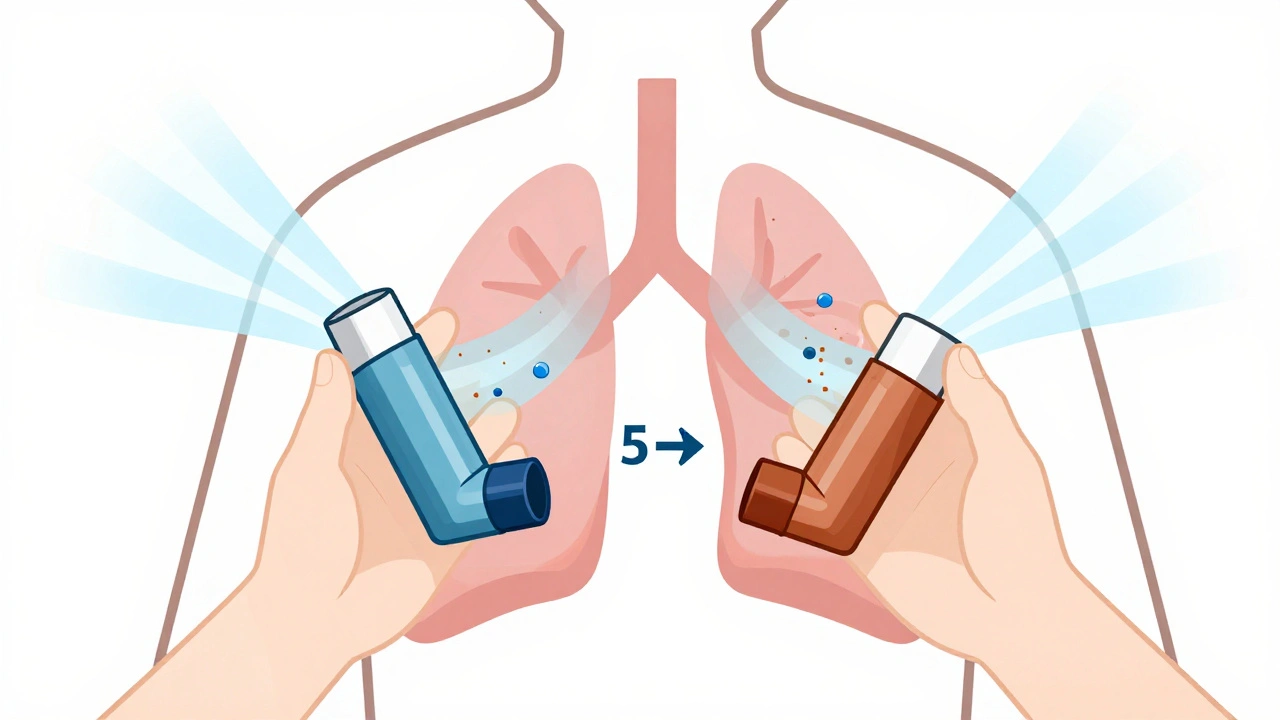
Why You Must Use Them in the Right Order
Here’s where most people mess up. You don’t just grab whichever inhaler is closest. The order matters. Every time.
Use your bronchodilator first. Wait five minutes. Then use your corticosteroid.
Why? Because inflamed airways are narrow. If you spray corticosteroid into a tight tube, most of it hits your throat and tongue. It doesn’t reach the small airways where inflammation lives. But when you open those airways with a bronchodilator first, the corticosteroid can travel deeper. Studies show this simple sequence increases drug delivery by up to 40%.
One Reddit user, "WheezingWarrior," put it plainly: "I didn’t realize how much better my breathing was until I started waiting 5 minutes between inhalers-my Pulmocort actually works now." That’s not luck. That’s science.
Hospitals and clinics now train patients on this sequence. Johns Hopkins found that when staff standardized this order, medication errors dropped by 47%. Yet, a 2023 Cleveland Clinic study showed 63% of patients still forget to wait. They rush. They mix them. They think it doesn’t matter. It does.

Combination Inhalers: The New Standard
Why carry two inhalers if you can carry one? That’s the logic behind combination inhalers like Advair (fluticasone + salmeterol), Symbicort (budesonide + formoterol), and Breo Ellipta (fluticasone + vilanterol). These devices deliver both drugs in a single puff.
They’re now used in 68% of asthma prescriptions in the U.S. That’s because they simplify treatment and reduce the chance of skipping the corticosteroid. The FACET trial showed Symbicort reduced asthma attacks by 29% compared to fluticasone alone.
And now there’s a new option: Airsupra. Approved by the FDA in 2023, it’s the first as-needed combination inhaler. It combines albuterol and budesonide in one device. You use it only when you feel symptoms-and you get both immediate relief and anti-inflammatory action in a single puff. GINA 2023 guidelines now recommend this for mild asthma instead of using SABA alone. Why? Because even occasional SABA use without anti-inflammatories increases long-term risk.
What You’re Probably Doing Wrong (And How to Fix It)
Here are the top mistakes people make-and how to avoid them:
- Mistake: Using your rescue inhaler more than 2-3 times a week. Fix: That’s a sign your asthma isn’t controlled. Talk to your doctor about adding or adjusting a corticosteroid.
- Mistake: Not rinsing after corticosteroids. Fix: Swish water in your mouth and spit. Do it every time. No exceptions.
- Mistake: Thinking your inhaler works the same every time. Fix: Technique matters. Only 31% of people use inhalers correctly without training. Ask your pharmacist to watch you. Use a spacer if you’re struggling.
- Mistake: Confusing your inhalers. Fix: Label them. Blue = rescue. Brown = daily. Write it on the cap if you have to.
A 2022 American Lung Association survey found only 47% of patients could correctly identify which inhaler was for emergencies and which was for daily use. That’s dangerous. If you’re using your rescue inhaler daily, you’re treating symptoms, not the disease. And you’re putting yourself at risk.

Side Effects You Need to Know About
Both types of inhalers have side effects-but they’re manageable.
With bronchodilators: You might feel jittery, have a fast heartbeat, or notice your hands shaking. That’s from the adrenaline-like effect. It usually fades after a few uses. If it doesn’t, talk to your doctor. Overuse can also make your body less responsive over time-some heavy users lose up to 50% of the drug’s effect.
With corticosteroids: Hoarseness, sore throat, and thrush are common. Rinsing helps. Long-term, high-dose use increases pneumonia risk in older COPD patients. But for most people, the benefits far outweigh the risks. The Cochrane Collaboration found inhaled steroids reduce exacerbations by 30%-and that’s life-saving.
What they don’t do: They don’t reverse lung damage in COPD. They don’t cure asthma. They don’t stop the disease from progressing. But they do stop it from getting worse. And that’s huge.
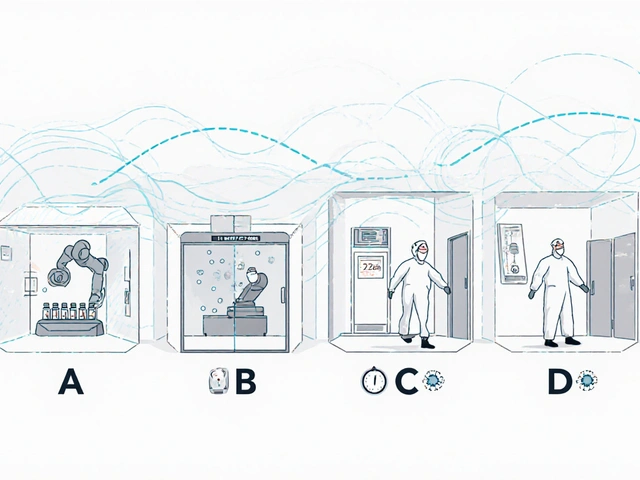
What’s Next for Respiratory Medications
The future is getting smarter. Doctors are starting to use FeNO tests-measuring nitric oxide in your breath-to see how much inflammation is present. That helps them decide exactly how much corticosteroid you need. No guessing.
Triple-therapy inhalers-combining a LABA, a LAMA (long-acting anticholinergic), and a corticosteroid-are now available. Trelegy Ellipta showed 25% fewer flare-ups than dual therapy in the TRIBUTE trial.
And there’s growing pressure to make inhalers greener. A single albuterol inhaler has the same carbon footprint as driving 300 miles. Dry powder inhalers (DPIs) are now 45% of new launches because they don’t use propellants. That’s a win for your lungs-and the planet.
One thing won’t change: the need for two tools. Bronchodilators for quick relief. Corticosteroids for long-term control. And the discipline to use them in the right order, at the right time.
Can I use a bronchodilator every day?
Short-acting bronchodilators like albuterol are meant for emergencies, not daily use. If you’re using your rescue inhaler more than 2-3 times a week, your asthma isn’t controlled. You likely need a daily inhaled corticosteroid. Using SABAs too often can make your body less responsive and increase your risk of severe attacks. Talk to your doctor if you’re relying on your blue inhaler regularly.
Why do I need to rinse my mouth after using a corticosteroid inhaler?
Corticosteroids can leave a small amount of medicine in your mouth and throat. That creates a moist environment where fungus can grow, leading to oral thrush-a white, sore coating in your mouth. Rinsing with water and spitting it out removes the residue and cuts your risk by more than half. Don’t swallow the rinse-just spit it out. This simple step prevents a common and avoidable side effect.
Do corticosteroids cure asthma or COPD?
No. Neither asthma nor COPD can be cured. Corticosteroids don’t reverse damage or stop the disease from progressing. But they do suppress inflammation, which reduces flare-ups, hospital visits, and long-term lung decline. For asthma, they’re the most effective long-term control medication available. For COPD, they help reduce exacerbations in people with frequent attacks. They’re not a cure-but they’re essential for staying well.
Is it safe to use combination inhalers like Advair or Symbicort long-term?
Yes, when used as directed. Combination inhalers are designed for daily use in people with persistent asthma or moderate-to-severe COPD. The FDA requires black box warnings because LABAs alone can increase death risk-but when paired with corticosteroids, that risk disappears. Millions use these safely for years. The key is taking them every day, even when you feel fine. Skipping doses is the biggest danger.
How do I know if my inhaler technique is correct?
Most people get it wrong. Signs of poor technique include the medicine hitting your tongue, throat, or cheeks instead of your lungs; not feeling the puff; or needing to use your inhaler more often than prescribed. Ask your pharmacist or respiratory therapist to watch you use it. Use a spacer if you’re struggling. Proper technique can double the amount of medicine reaching your lungs. The American Lung Association offers free video tutorials online-watch them, then practice in front of a mirror.
If you’re using bronchodilators and corticosteroids correctly, you’re not just managing symptoms-you’re protecting your lungs for years to come. It’s not complicated. It’s just simple. And it only works if you do it right, every time.


Michael Robinson
December 10, 2025 AT 09:33It’s wild how something so simple-rinse and wait five minutes-can change your whole life. I used to rush through my inhalers like they were coffee shots. Then one day, my lungs actually felt like they belonged to me again. No magic pills. Just dumb, boring discipline.
People act like medicine is a hack, but it’s really just showing up every day and doing the thing you don’t feel like doing. That’s the real treatment.
And yeah, I still shake after my albuterol. But I’d rather shake than suffocate.
Kathy Haverly
December 12, 2025 AT 05:46Oh please. This is just pharmaceutical propaganda dressed up as ‘science.’ You think the lung is some delicate flower that needs a daily spray of chemicals to survive? My grandpa had asthma in the 70s and never used a corticosteroid. He smoked, drank, and still lived to 89. Your ‘control’ is just corporate greed with a stethoscope.
And don’t get me started on ‘combination inhalers.’ They’re just a way to make you buy two drugs as one overpriced box. You’re being trained to be a lifelong customer, not a healthy person.
Also, why is everyone suddenly obsessed with ‘technique’? My neighbor’s dog inhales better than I do, and she’s fine.
Evelyn Pastrana
December 13, 2025 AT 04:48Okay but can we talk about how the fact that we’re even having this conversation is kind of tragic? Like, we’ve got people dying because they don’t know to rinse their mouth after using an inhaler. That’s not a medical failure-that’s a societal failure.
Imagine if we taught this in middle school. Not just ‘don’t touch the stove,’ but ‘here’s how to keep your lungs from turning into a brick.’
Also, I love that Airsupra exists now. It’s like someone finally said, ‘Hey, what if we just… made the right thing easier?’
And yes, I’m the person who rinses after every puff. And yes, I still feel weird about it. But I’d rather be weird than in the ER again.
Also, the carbon footprint thing? Mind blown. I’m switching to a DPI now. My lungs and the planet can both breathe easier.
Also also, I just told my 12-year-old cousin all this. She’s gonna teach her teacher. Small wins, people.
Nikhil Pattni
December 14, 2025 AT 21:30Bro I am from India and we don't have access to all these fancy inhalers like Advair or Symbicort, we use only Budecort and Asthalin, and still we manage. In my village, people use nebulizers with saline and salbutamol, and they live. You Americans think you need all this high-tech stuff but actually the core is simple: keep airways open, reduce inflammation.
Also, I read in a study that 80% of asthma deaths in developing countries are due to lack of access, not misuse. So stop acting like your technique is the only thing that matters. My cousin died because he couldn't afford a spacer, not because he didn't rinse his mouth.
And yes, I use emoticons: 😔
Also, I asked my doctor about FeNO test and he laughed. Said we don't have the machine. So what do we do? We use what we have. And we survive.
Also, my neighbor uses a plastic bottle as a spacer. It works. No need for $50 devices. Just clean bottle, cut bottom, put inhaler in, breathe. Simple. Human.
Also, I think the real problem is not the inhalers-it's the doctors who don't take time to teach. I had to learn all this from YouTube. Not from my pulmonologist. Sad.
Also, I am not exaggerating. I have 14 years of asthma. I know.
Arun Kumar Raut
December 15, 2025 AT 20:41Hey everyone, I just want to say this post was really helpful-and I mean that. I’ve been using my inhalers wrong for years, and I didn’t even know it. I thought the blue one was just for when I felt bad, and the brown one was… optional. Turns out, I was just surviving, not living.
So I started rinsing. I started waiting five minutes. I labeled my inhalers with colored tape. And guess what? I haven’t used my rescue inhaler in three weeks.
I’m not a doctor. I’m not a scientist. I’m just someone who got tired of waking up coughing. If I can change, anyone can.
And if you’re struggling with the cost? Talk to your pharmacist. There are patient assistance programs. I got my Symbicort for $10 a month through one. It’s out there.
Also, don’t be ashamed if you need help. I asked my cousin to watch me use it. Felt dumb. Now I feel proud.
We’re all in this together. No one should have to breathe like they’re underwater.
precious amzy
December 17, 2025 AT 11:08One must question the epistemological foundations of this narrative. The entire discourse on bronchodilators and corticosteroids is predicated upon a biomedical paradigm that pathologizes normal physiological variation. The notion that ‘inflammation’ must be suppressed at the genetic level is a reductionist fantasy engineered by Big Pharma to sustain perpetual dependency.
Furthermore, the recommendation to ‘rinse after use’ is a performative gesture-a ritual of compliance that distracts from the deeper issue: why are we being medicated for environmental degradation, poor urban planning, and systemic neglect?
The ‘SMART trial’ cited is funded by GlaxoSmithKline. The FACET trial? Sponsored by AstraZeneca. The ‘science’ here is not science-it is institutionalized rhetoric.
And yet, you all nod along. You rinse. You wait. You buy. You obey. The real tragedy is not asthma. It is the surrender of critical thought to the altar of medical authority.
Perhaps, instead of inhalers, we ought to cultivate silence. And stillness. And air free of particulates. But no-better to buy another device.
-P.S. I do not use inhalers. I meditate. And I breathe. Deeply.
William Umstattd
December 19, 2025 AT 08:38You people are ridiculous. You treat asthma like it’s a yoga class where you need the right mat and the perfect sequence. It’s a chronic illness. You don’t get bonus points for rinsing your mouth. You don’t get a medal for waiting five minutes. You just don’t die.
And let’s be real-most of you are just following instructions because you’re too scared to ask the real question: ‘Why am I still having attacks?’
My cousin had asthma since birth. Used every inhaler known to man. Still ended up in ICU twice. No amount of ‘technique’ fixes a broken system.
Stop pretending this is about discipline. It’s about luck. Luck that your insurance covers it. Luck that your doctor didn’t dismiss you. Luck that you weren’t born in a place where ‘inhaler’ means a luxury.
And if you think this post is helpful? Congrats. You’re the kind of person who thinks reading a manual makes you an expert.
Go breathe.
Elliot Barrett
December 20, 2025 AT 23:05I used to use my rescue inhaler every day. Now I use it once a month. All I did was rinse. No magic. Just spit out the water. I’m not even kidding.
Also, I didn’t know I was supposed to wait five minutes. I thought it was a myth. Turns out it’s not.
Thanks for the reminder, I guess.