Long-term steroid use can silently damage your eyes-here’s how to protect your vision
If you’ve been on steroids for months-whether as eye drops, pills, inhalers, or injections-you might think the biggest risks are weight gain, mood swings, or high blood sugar. But there’s another danger hiding in plain sight: your eyes. Steroids are powerful anti-inflammatory drugs, but they don’t just calm down your immune system. They can also trigger two serious, vision-threatening conditions: steroid-induced cataracts and steroid-induced glaucoma. And here’s the scary part: you might not notice anything wrong until it’s too late.
Unlike the slow, gradual vision loss from aging, steroid-related eye damage can happen fast. Some people develop cloudy lenses or rising eye pressure after just a few weeks of use. The good news? These problems are often preventable-if you know what to watch for and how to act.
How steroids turn your eyes into a ticking time bomb
Steroids don’t just float around your body. Once they enter your system, they interact with tissues in your eyes in ways that change how they work. For your lens, steroids trigger a chemical reaction that builds up abnormal proteins. These proteins clump together and cloud the lens, forming what’s called a posterior subcapsular cataract. This isn’t the kind of cataract you get from aging. It forms at the back of the lens, right where light focuses, so it messes with your vision faster and more severely.
One patient on Reddit shared their story: after six months of prednisone for asthma, their vision dropped to 20/80. They had no symptoms-no pain, no blurry vision they could explain-until their eye exam showed advanced cataracts. That’s how sneaky this is.
For glaucoma, the problem is pressure. Steroids block the drainage channels in your eye that normally let fluid out. When that fluid builds up, pressure inside your eye rises. This is called intraocular pressure (IOP). High IOP crushes the optic nerve over time, and once that nerve dies, you lose vision forever.
Here’s the twist: not everyone reacts the same way. About 5% of people are extreme responders-they see their eye pressure jump 15 mmHg or more with even short steroid use. Another 30% have moderate rises. And then there’s the rest. The problem? You won’t know which group you’re in until it’s too late.
Who’s most at risk-and why
Some people are walking time bombs for steroid eye damage, even if they’ve never had eye problems before. The biggest risk group? People with a family history of glaucoma. If your parent or sibling has it, your odds of developing steroid-induced glaucoma jump dramatically.
People who already have glaucoma? Nearly 90% of them become steroid responders. That means even a single drop of steroid eye drops can send their pressure soaring. This is why doctors avoid prescribing steroids to glaucoma patients unless there’s no other option.
Another high-risk group: those who’ve had cataract surgery. After surgery, doctors often prescribe steroid eye drops to reduce swelling. But in up to 40% of these cases, the drops trigger new pressure spikes. Many patients don’t realize the connection until they start losing peripheral vision.
And here’s something most people don’t know: steroid-induced glaucoma shows up in people with no prior eye history nearly 35% of the time. That means if you’ve never had an eye exam in your life, and you’re on long-term steroids, you’re still at risk.
The difference between steroid cataracts and regular cataracts
Not all cataracts are the same. Age-related cataracts form slowly over years. They start with mild blurriness, then gradually make colors look faded and lights seem too bright. Steroid-induced cataracts? They’re different. They grow faster, start at the back of the lens, and cause problems with glare and night vision almost immediately.
Think of it like this: if age-related cataracts are a slow leak in your car’s tire, steroid cataracts are a blowout. You might be driving fine one day, then suddenly you’re struggling to see the road ahead-even with your glasses on.
Patients often describe it as seeing halos around lights, colors looking washed out, or trouble driving at night. One Healthgrades review said: “I didn’t realize my steroid eye drops for uveitis were causing glaucoma until I lost peripheral vision-now I need multiple daily eye drops permanently.”
Because these cataracts progress faster, surgery is often needed sooner. And unlike age-related cataracts, which are common in older adults, steroid cataracts can hit people in their 30s, 40s, or 50s-long before they’d normally expect vision problems.

How steroid glaucoma differs from regular glaucoma
Regular glaucoma, called primary open-angle glaucoma (POAG), develops slowly. It’s often called the “silent thief of sight” because it steals your peripheral vision without warning. Steroid-induced glaucoma looks the same on the outside-but the cause is different.
The biggest difference? Reversibility. If you stop the steroids early enough, your eye pressure often drops back to normal. The optic nerve can recover. But if you wait too long, the damage becomes permanent. That’s why timing matters more than anything.
Here’s what the data says: in most cases, IOP rises by less than 5 mmHg. That’s not alarming. But in 30% of cases, it jumps 6-15 mmHg. And in 5% of cases? It shoots up over 15 mmHg. That’s enough to cause nerve damage in weeks.
And unlike POAG, which is lifelong, steroid glaucoma can be reversed-if caught early. But if you ignore it, it turns into permanent glaucoma. And once it does, you’re stuck with daily eye drops, laser treatments, or even surgery for the rest of your life.
What forms of steroids are most dangerous for your eyes
Not all steroid use is created equal when it comes to eye risk. Topical steroid eye drops are the most dangerous because they go straight into your eye. One drop a day for a month can be enough to trigger high pressure or cataracts in a sensitive person.
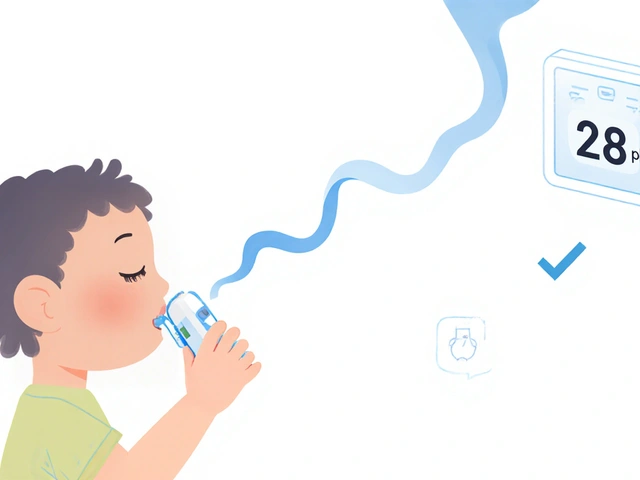
Oral steroids like prednisone are next on the list. It takes longer-usually 2 to 4 weeks of daily use-to cause eye damage. But once it starts, it’s just as serious. Inhaled steroids (like asthma inhalers) carry lower risk, but they’re not safe. The steroids can still get into your bloodstream and reach your eyes.
Injectable steroids, like those given for joint pain or autoimmune conditions, also pose a threat. Even a single shot can cause a spike in eye pressure in high-risk people.
Here’s a hard truth: if you’re on steroids for more than 2-4 weeks, you’re in the danger zone. The longer you use them, the higher your risk. And the more often you use them-even in small doses-the more your eyes get exposed.
How to protect your eyes if you’re on steroids
You don’t have to stop your medication. But you do need to protect your eyes. Here’s what works:
- Get a baseline eye exam before starting steroids. This includes measuring your eye pressure and checking the health of your optic nerve and lens. If you already have glaucoma or cataracts, your doctor needs to know.
- Get checked every 2 weeks for the first 2 months. Then every 4-6 weeks for the next 3 months. If your pressure stays normal, you can switch to every 6 months. But don’t skip these visits.
- Use the lowest dose possible for the shortest time. Ask your doctor: “Is there a non-steroid alternative?” Sometimes, newer anti-inflammatories like loteprednol etabonate can do the job with less risk.
- Know the warning signs. Halos around lights, faded colors, blurry vision, eye pain, redness, or trouble seeing at night? Don’t wait. Get checked.
- Don’t assume your primary care doctor will refer you. Only 42% of primary care doctors routinely refer long-term steroid users to an eye specialist. You have to ask.
Some clinics now offer home IOP monitoring devices for high-risk patients. These are small, handheld tools that let you check your eye pressure at home and send the data to your doctor. It’s not perfect-but it’s better than waiting until your vision is already damaged.

What to do if you’ve already been on steroids for months
If you’ve been on steroids for more than 2 months and haven’t had an eye exam, don’t panic-but don’t wait either. Schedule an appointment with an ophthalmologist right away. Bring a list of every steroid you’ve taken, including doses and how long you used them.
If your pressure is high but your optic nerve looks fine, stopping the steroid may be enough. Your pressure could drop back to normal in weeks. But if there’s already nerve damage, you’ll need glaucoma treatment-eye drops, laser therapy, or surgery-to prevent further loss.
For cataracts, surgery is the only fix. But if caught early, it’s a simple, safe procedure with a high success rate. The key is catching it before it makes daily life impossible.
What’s changing in eye care for steroid users
Doctors are getting smarter about this. New research from March 2024 found genetic markers that can predict who’s likely to be a steroid responder-with 85% accuracy. That means in the near future, a simple blood test could tell you if you’re at high risk before you even start steroids.
Tele-ophthalmology is also growing. The Veterans Health Administration tested remote eye monitoring for 27,000 steroid users. Patients used apps to report symptoms and sent photos of their eyes. It worked. Early detection improved. Vision loss dropped.
And new steroid eye drops are being developed that are just as effective at reducing inflammation-but much less likely to raise eye pressure. One study in JAMA Ophthalmology found loteprednol etabonate caused significantly less pressure rise than older steroids.
The message is clear: steroid eye damage isn’t inevitable. It’s preventable-with the right knowledge, the right checks, and the right questions.
Don’t let steroids steal your sight
Steroids save lives. They control asthma, reduce swelling after surgery, calm autoimmune flare-ups. But they’re not harmless. Your eyes are paying a price you might not even know about.
There’s no shame in needing steroids. But there’s real danger in ignoring your eyes. The best defense isn’t fear-it’s awareness. Know your risk. Get checked. Ask questions. Don’t wait for blurry vision or tunnel vision to sound the alarm.
Because when it comes to your eyes, early action doesn’t just help-it can save your vision.
Can steroid eye drops cause cataracts and glaucoma?
Yes. Steroid eye drops are one of the most common causes of steroid-induced eye damage. Because they’re applied directly to the eye, they can trigger both posterior subcapsular cataracts and elevated intraocular pressure (glaucoma) in as little as 2-4 weeks. Even a single drop daily can be enough for sensitive individuals.
How long does it take for steroids to damage your eyes?
It varies. For eye drops, damage can start in 2-4 weeks. For oral steroids like prednisone, it usually takes 4-8 weeks of daily use. But in high-risk people-those with a family history of glaucoma or existing eye conditions-it can happen even faster. There’s no safe timeline; only a risk timeline.
Is steroid-induced glaucoma reversible?
Yes-if caught early. When steroid use stops, eye pressure often returns to normal within weeks. But if the pressure stays high for months, it can permanently damage the optic nerve. Once the nerve is damaged, vision loss is irreversible. That’s why timing is everything.
Can you get steroid eye damage without symptoms?
Absolutely. Steroid-induced glaucoma is called the "silent thief of sight" because it often causes no pain or obvious symptoms until peripheral vision is already lost. Cataracts from steroids can also develop without warning. That’s why regular eye exams are critical-even if you feel fine.
Should I stop taking steroids if I’m worried about my eyes?
Never stop steroids without talking to your doctor. Suddenly stopping can cause dangerous side effects like adrenal crisis. Instead, ask your doctor about eye monitoring, lowering your dose, or switching to a safer alternative. The goal is to balance your health needs with eye safety-not to quit treatment cold turkey.
Are there steroid alternatives that are safer for the eyes?
Yes. Newer steroid eye drops like loteprednol etabonate are designed to be just as effective at reducing inflammation but much less likely to raise eye pressure. For systemic use, non-steroid anti-inflammatories like NSAIDs or biologics may be options depending on your condition. Always discuss alternatives with your doctor.
How often should I get my eyes checked if I’m on long-term steroids?
The American Academy of Ophthalmology recommends: baseline exam before starting, then every 2 weeks for the first 2 months, then every 4-6 weeks for 3 months. If your pressure stays normal, you can switch to every 6 months. But if you’re high-risk-family history of glaucoma, previous eye surgery, or using high-dose drops-your doctor may want you checked more often.
Can children develop steroid-induced eye damage?
Yes. Children on long-term steroid therapy-for asthma, allergies, or autoimmune diseases-are at risk too. Their eyes are still developing, so damage can progress faster. Pediatric ophthalmologists recommend baseline eye exams and regular monitoring for any child on steroids for more than 2 weeks.






swatantra kumar
November 20, 2025 AT 22:25Rebecca Cosenza
November 22, 2025 AT 01:41Cinkoon Marketing
November 23, 2025 AT 00:09And yeah, your PCP won't tell you. They're not eye doctors. You have to push. Ask for the tonometer. Demand the baseline. If they roll their eyes, go elsewhere.
Bill Camp
November 23, 2025 AT 12:31Nick Naylor
November 24, 2025 AT 22:03Lemmy Coco
November 26, 2025 AT 04:17Brianna Groleau
November 26, 2025 AT 22:24If you have family history? Don't wait. Don't hope. Don't assume. Act. Your future self will thank you.
Dave Wooldridge
November 28, 2025 AT 07:51They want you scared of your own immune system. They want you dependent. They want you blind - but still paying for drops.
Check your eye pressure. Then check who owns the company that makes your drops. You’ll see the pattern.
Sarah Swiatek
November 29, 2025 AT 07:37Turns out, I’m one of those 5% extreme responders. My doctor said if I’d waited another month, I’d have permanent damage.
So now I tell everyone: if you’re on steroids - even for a week - get your eyes checked. It takes 10 minutes. It could save your life.
serge jane
November 29, 2025 AT 11:32There’s no moral failing in needing steroids. There’s no weakness in asking for monitoring. What’s weak is pretending we can outsmart biology with optimism. We need humility. We need science. We need routine.
Rusty Thomas
November 29, 2025 AT 13:51Matthew McCraney
December 1, 2025 AT 06:28So they give you pamphlets. They say 'be aware.' They don’t give you a blood test. They don’t give you a mandatory scan. They don’t even require the pharmacy to print a warning on the label.
It’s not an oversight. It’s a cover-up.