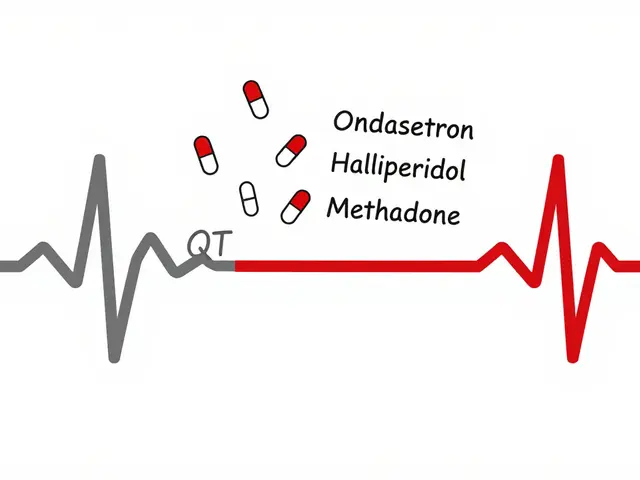
Imagine you’re a pharmacist. A patient walks in with a new prescription for blood pressure medication. You check their history, notice they’re already on three other drugs, and spot a dangerous interaction. But you can’t see their latest lab results, their doctor’s notes, or whether they filled the last prescription. You guess. You call the clinic. You wait. This is still the reality for most independent pharmacies in 2026 - EHR integration is the exception, not the rule.
Why EHR Integration Matters More Than Ever
Electronic Health Record (EHR) integration between doctors and pharmacies isn’t just tech buzzword. It’s the difference between a patient getting the right meds and ending up back in the hospital. When systems talk to each other, pharmacists can see real-time data: recent lab values, allergies, previous prescriptions, even notes from specialists. That’s not convenience - it’s safety. In 2021, a study in East Tennessee showed that when pharmacies using PioneerRx software could access Epic EHR data, they caught and fixed 1,847 medication issues in just a few months. Providers accepted 92% of those suggestions. That’s not magic. That’s data. The numbers don’t lie. Integrated systems reduce medication errors by 48%, cut prescription processing time from 15 minutes to under 6 minutes, and lower hospital readmissions by 31%. In Australia, the My Health Record system cut preventable hospitalizations by 27%. These aren’t hypothetical gains. They’re happening - but only where integration exists.How EHR and Pharmacy Systems Actually Talk
It’s not plug-and-play. Pharmacy and provider systems speak different languages. The bridge? Two main standards: NCPDP SCRIPT and HL7 FHIR. NCPDP SCRIPT (version 2017071) handles the actual prescription - what drug, dose, instructions, refill rules. It’s been around since the 90s and still carries 97% of electronic prescriptions in the U.S., mostly through Surescripts. But SCRIPT alone can’t tell a pharmacist if the patient’s kidney function dropped last week or if their heart failure worsened. That’s where HL7 FHIR (Fast Healthcare Interoperability Resources) comes in. FHIR lets systems share clinical data: lab results, diagnoses, care plans, even patient-reported symptoms. The Pharmacist eCare Plan (PeCP), built on FHIR, lets pharmacists send structured notes back to the provider’s EHR - like, “Patient couldn’t afford med, switched to generic, BP improved.” These standards work together. SCRIPT sends the script. FHIR sends the context. Surescripts, which processes over 22 billion transactions yearly, connects most of this traffic. But only 15-20% of U.S. pharmacies have true bidirectional integration - meaning they can both send and receive full clinical data.Who’s Getting It Right - And Who’s Left Behind
There’s a huge gap. Hospitals and big health systems? 89% have EHR integration with their in-house pharmacies. Their systems are built on the same platform - Epic, Cerner, Meditech - so sharing data is easier. Independent pharmacies? Only 12% do. Why? Cost. A small pharmacy might spend $15,000 to $50,000 just to get connected. Then $5,000-$15,000 a year to keep it running. For a single-owner shop, that’s not an IT expense - it’s a survival risk. Even if they pay, they often can’t get access. In Wisconsin, researchers found only 3 out of 127 community pharmacies had formal agreements with local health systems. That’s less than 0.01% of the state’s pharmacists. Meanwhile, Surescripts and SmartClinix offer solutions, but they’re not cheap. SmartClinix starts at $199/month per provider. DocStation is $249/month. For a small pharmacy with two pharmacists and three techs, that’s over $6,000 a year just for software. And then there’s the human side. Pharmacists average 2.1 minutes per patient. That’s not enough time to dig through EHR data, even if they can see it. A 2021 Ohio State survey found 68% of pharmacists feel they don’t have time to use EHR tools properly. They’re drowning in alerts, not empowered by insights.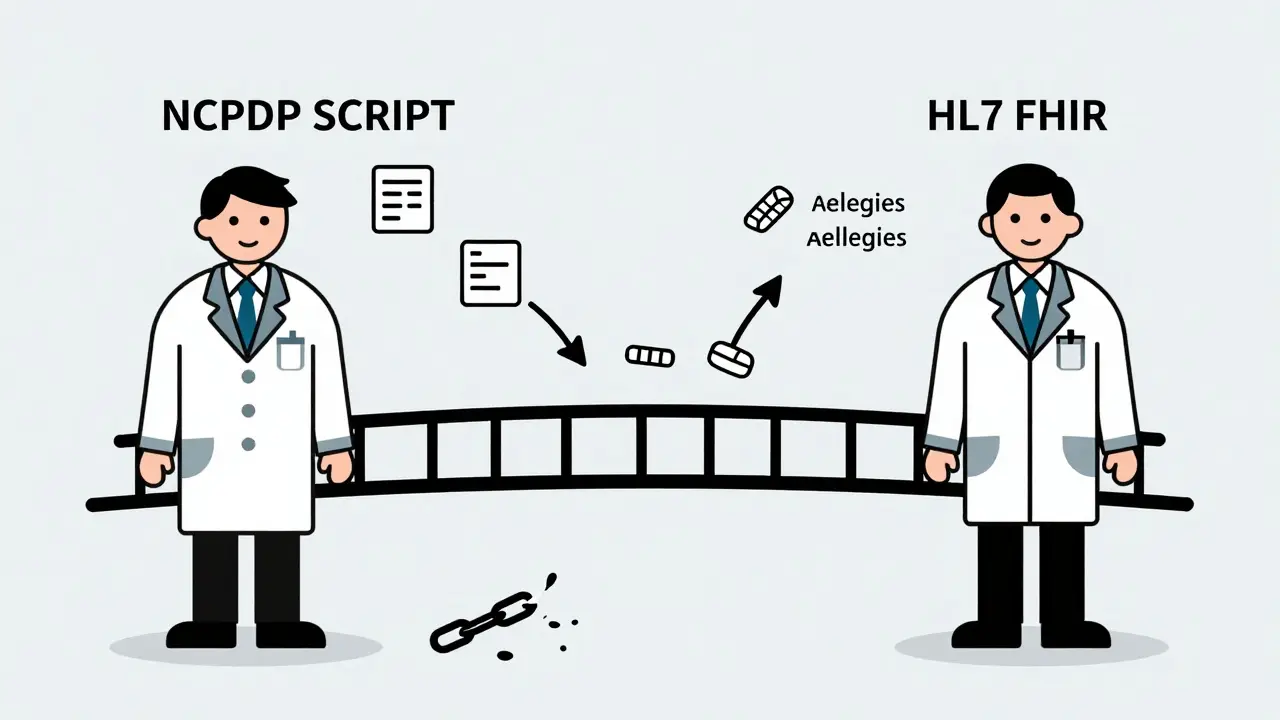
The Hidden Costs - Time, Training, and Trust
Integration isn’t just about buying software. It’s about changing how people work. First, training. Pharmacists need to understand FHIR data structures, interpret clinical notes, and know when to act. A 2022 AMIA survey said change management was “essential” for 64% of successful projects. But most training is rushed - often just a 90-minute webinar. Second, data mapping. There are over 120 EHR systems and 50 pharmacy platforms in the U.S. Getting them to talk means translating messy, inconsistent data. One system calls it “hypertension,” another says “HTN.” One sends labs in PDFs, another in structured tables. That’s 20-40 hours of manual cleanup per integration. Third, trust. Providers don’t always trust pharmacist notes. “Is this just a billing ploy?” some doctors wonder. But when pharmacists use PeCP to send clear, evidence-based interventions - like “Patient’s HbA1c dropped from 8.9 to 7.1 after switching meds and adding counseling” - providers start listening. The key? Structure. Clarity. Evidence.What’s Changing in 2026 - And What’s Still Broken
The tide is turning - slowly. The 21st Century Cures Act banned “information blocking” in 2021. That means providers can’t legally refuse to share data with pharmacies. CMS now requires Medicare Part D plans to integrate medication therapy management (MTM) by 2025. California’s SB 1115 mandates EHR integration for MTM by 2026. These aren’t suggestions - they’re rules. The Office of the National Coordinator for Health IT now lists pharmacy integration as a “Tier 1” priority, with a goal of 50% of community pharmacies having bidirectional access by 2027. That’s ambitious - but possible. New tools are emerging. CARIN Blue Button 2.0 lets patients download their own data from insurers and send it directly to their pharmacy. AI pilots by CVS and Walgreens are using machine learning to flag high-risk patients before they even walk in - identifying 37% more issues than humans alone. But here’s the catch: payment. Only 19 states reimburse pharmacists for EHR-based care coordination. Even though 48 states let pharmacists prescribe, they can’t get paid for using the data they’re given. As Dr. Lucinda Maine of the American Association of Colleges of Pharmacy put it: “Without sustainable payment models, EHR integration will remain a luxury.”
What You Can Do - Even If You’re a Small Pharmacy
You don’t need to be Epic to benefit. Start small.- Use Surescripts’ Medication History service - it’s free for most pharmacies and gives you access to 3.5 billion annual prescription records.
- Ask your EHR vendor if they support FHIR APIs. If not, push them. Demand it.
- Join a local pharmacy coalition. Shared resources reduce costs. In Ohio, 12 small pharmacies pooled funds to integrate with one health system - cutting individual costs by 60%.
- Start documenting your interventions. Even if you can’t send them to the EHR yet, write them down. Show your value. Providers notice when you prevent a hospital stay.
Real Impact, Real Stories
One pharmacist in Tennessee used integrated data to catch a patient’s dangerously low potassium level - a side effect of a new diuretic. The doctor hadn’t seen the lab. The patient was asymptomatic. But the pharmacist saw it. They called. The dose was adjusted. No ER visit. No $12,000 hospital bill. Another in California used FHIR to see that a patient was filling a new opioid script while still on a high-dose benzodiazepine. She flagged it. The provider changed the plan. The patient didn’t overdose. These aren’t rare. They’re routine - but only where integration exists.The Future Is Connected
EHR integration isn’t about technology. It’s about respect. It’s saying: pharmacists aren’t just dispensers. We’re clinicians. We’re on the front lines. We see the whole picture. The tech is here. The data is available. The proof is in the numbers: fewer errors, fewer hospitalizations, lower costs, better outcomes. The only thing missing? Willingness to pay for it. To train for it. To trust it. If your pharmacy hasn’t integrated yet, you’re not behind. You’re just waiting. And every day you wait, someone risks a preventable mistake.What is EHR integration in pharmacy?
EHR integration in pharmacy means connecting a pharmacy’s system directly with a doctor’s Electronic Health Record (EHR). This allows pharmacists to see patient data like lab results, allergies, and other prescriptions - and send back clinical notes about medication changes or risks. It’s bidirectional communication that helps prevent errors and improve care.
How does EHR integration reduce medication errors?
Integrated systems automatically flag dangerous drug interactions, duplicate prescriptions, or incorrect doses based on real-time patient data. Studies show this cuts medication errors by up to 48%. For example, a pharmacist can see that a patient is already on a blood thinner and catch a new prescription that could cause dangerous bleeding.
Why don’t more pharmacies have EHR integration?
Cost is the biggest barrier. Independent pharmacies face $15,000-$50,000 in setup fees and $5,000-$15,000 yearly in maintenance. Many also lack time, training, or access agreements with health systems. Only 12% of independent U.S. pharmacies have full integration as of 2026.
What standards do pharmacies use for EHR integration?
The two main standards are NCPDP SCRIPT (for sending prescriptions) and HL7 FHIR (for sharing clinical data like lab results and care plans). FHIR allows pharmacists to send structured notes back to providers through the Pharmacist eCare Plan (PeCP), turning them into active care team members.
Can patients help with EHR integration?
Yes. Through CARIN Blue Button 2.0, patients can download their own prescription and lab data from insurers and send it directly to their pharmacy. This helps fill gaps when provider systems aren’t connected - especially for patients seeing multiple doctors.
Is EHR integration required by law?
Not yet for all pharmacies, but regulations are pushing hard. The 21st Century Cures Act bans information blocking. Medicare Part D requires MTM integration by 2025. California mandates it for MTM by 2026. The federal goal is 50% of community pharmacies integrated by 2027.





Darren McGuff
January 9, 2026 AT 06:16Let’s be real - this isn’t about tech, it’s about power. Pharmacies have been the unsung heroes of primary care for decades, but the system still treats them like order-takers. FHIR and SCRIPT? Great. But until payers start reimbursing for clinical time, not just pills, we’re just decorating a sinking ship. 🤷♂️
Patty Walters
January 10, 2026 AT 08:44i’ve been in this game 18 yrs and i still get calls like ‘can you just check if this med is okay?’ with no labs, no history… it’s wild. we’re not magic. we’re just the last line before someone ends up in the er. if my ehr could just show me the last creatinine, i’d sleep better. 😔
Gregory Clayton
January 12, 2026 AT 01:34Oh here we go again. Another ‘pharmacists are clinicians’ lecture. Newsflash: you don’t get to write prescriptions in most states, and you’re not reading MRIs. Stop pretending you’re a doctor. Just fill the script and let the MDs do their job. 🤦♂️
Matthew Maxwell
January 12, 2026 AT 12:23It is a profound moral failure that a nation which spends over $4 trillion annually on healthcare cannot ensure that a pharmacist, standing at the front line of medication safety, has access to basic clinical data. This is not inefficiency - it is institutional negligence. The fact that we still rely on fax machines and verbal handoffs in 2026 is a national disgrace. The technology exists. The will does not. And therein lies the tragedy.
Chris Kauwe
January 13, 2026 AT 13:31Let’s cut through the FHIR buzzword bingo. NCPDP SCRIPT is the backbone - it’s been working since the 90s. FHIR? It’s the shiny new toy that’s bloating workflows with JSON schemas and ‘interoperability’ theater. Meanwhile, the guy at the counter still has to call three clinics to find out if the patient actually took the last dose. Stop over-engineering. Fix the damn pipeline. The real innovation is not in APIs - it’s in giving pharmacists five extra minutes per patient to actually talk to them.
Maggie Noe
January 14, 2026 AT 18:40Imagine if your car’s GPS could only see the road you were on… but not the traffic ahead, the weather, or the fact that your tire was flat. That’s what pharmacy systems are like. We have the maps. We have the sensors. But no one lets us use them. 🚗💨 I’m tired of being the only one who sees the crash coming and having no way to warn anyone. #PharmacistsAreClinicians
Kiruthiga Udayakumar
January 14, 2026 AT 23:25As someone from India where we have 100+ pharmacies sharing one EHR server (yes, really), I can tell you - it’s not about the tech, it’s about trust. In the U.S., you have the money. You have the standards. You just don’t have the humility to let pharmacists speak. We fix 70% of errors before they happen. Why are we still asking for permission to help?
Jenci Spradlin
January 16, 2026 AT 09:58my boss says we can’t afford smartclinix. so i use free surescripts med history + a google sheet i made to track med conflicts. it’s janky as hell but saved 3 people this month. if you’re a small shop, don’t wait for the system to save you. just start documenting. one note at a time. you’ll be shocked who starts listening.
Heather Wilson
January 17, 2026 AT 01:50Let’s analyze the data: 12% integration rate among independents. That’s 88% of pharmacies operating in a state of near-constant clinical risk. The cost of integration? $15k–$50k. The cost of a single preventable hospitalization? $12k–$150k. The cost of a patient death? Unquantifiable. So why are we still debating budgets? This isn’t a cost problem - it’s a moral accounting failure. And someone needs to be held accountable.
Jeffrey Hu
January 18, 2026 AT 16:22Everyone’s talking about FHIR like it’s the holy grail, but nobody mentions that 70% of EHRs still don’t support it properly. And Surescripts? They’re a monopoly disguised as a utility. The real problem isn’t integration - it’s vendor lock-in. If you want real change, stop begging for access and start demanding open APIs. Or better yet - build your own. I did. Took me 6 months. Worth it.
Micheal Murdoch
January 19, 2026 AT 04:16Hey - if you’re a small pharmacy reading this and thinking ‘I can’t do this’ - you already are. Every time you catch a bad interaction without the system? That’s integration. Every time you write down a note and hand it to the doctor? That’s PeCP. You’re already the care team. The tech just needs to catch up. Don’t wait for permission. Just keep showing up. One patient. One script. One saved life at a time. You’re not behind. You’re already winning.
Catherine Scutt
January 21, 2026 AT 03:24Ugh. Another ‘pharmacist hero’ post. Look, I get it - you’re tired of being treated like a robot. But let’s not pretend every pharmacist wants to be a clinician. Some of us just want to count pills and get home. Stop romanticizing burnout. Not everyone wants to be a data analyst with a white coat.
Ashley Kronenwetter
January 22, 2026 AT 02:46Thank you for this comprehensive overview. The data presented is compelling, and the distinction between NCPDP SCRIPT and HL7 FHIR is clearly articulated. I would only add that the regulatory momentum described - particularly under the 21st Century Cures Act and California SB 1115 - represents a necessary and overdue correction to systemic fragmentation. The next phase must focus on standardizing clinical terminology across platforms to reduce mapping overhead. This is not merely technical - it is a foundational requirement for equitable care.