IPF Treatment Decision Calculator
When treating idiopathic pulmonary fibrosis (IPF), Esbriet (Pirfenidone) is a oral anti‑fibrotic medication approved by the FDA to slow disease progression. Patients often wonder how it stacks up against other options. This guide walks through the science, dosing, safety profile, cost, and real‑world experience so you can decide if Esbriet vs alternatives is the right conversation for you.
What is Idiopathic Pulmonary Fibrosis?
Idiopathic Pulmonary Fibrosis is a chronic, progressive scarring of the lung tissue that impairs oxygen transfer. The cause is unknown, hence “idiopathic.” It typically affects adults over 60 and shortness of breath is the hallmark symptom. Without treatment, median survival is 3‑5 years after diagnosis.
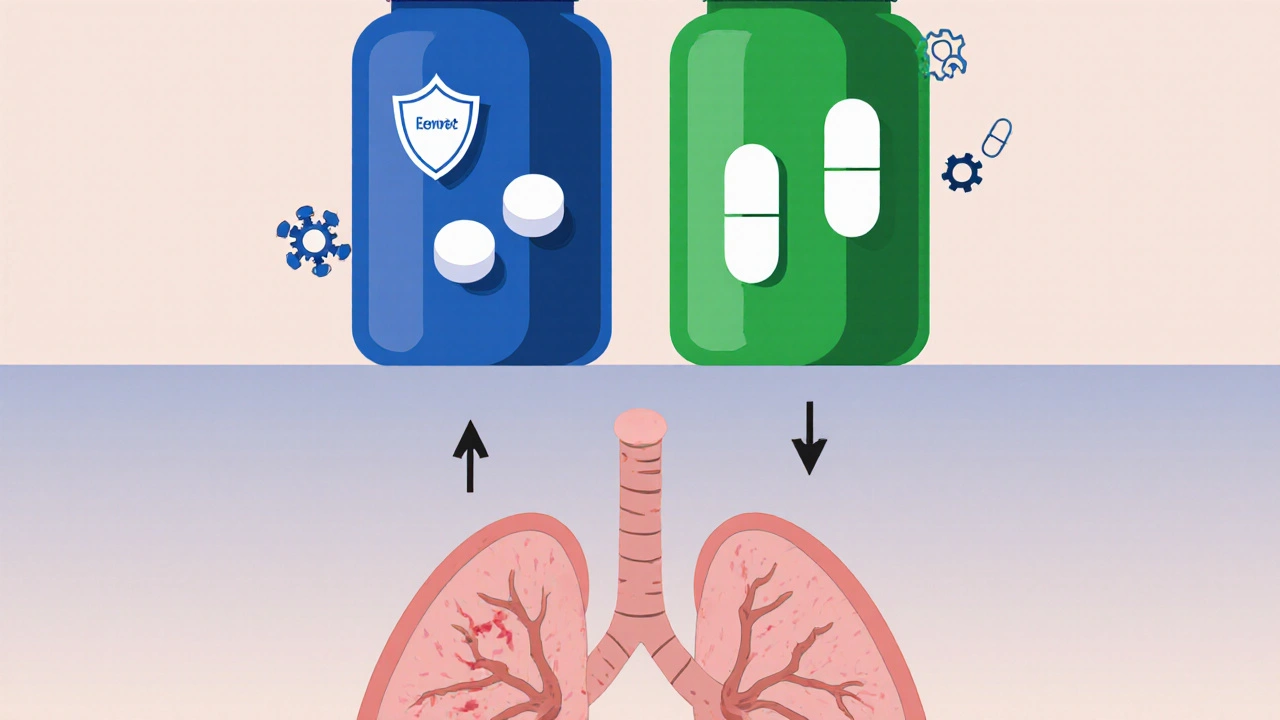
How Esbriet Works
Esbriet belongs to the class of anti‑fibrotic agents, which interfere with the pathways that lead to collagen deposition. Laboratory studies show Pirfenidone (the active ingredient) reduces fibroblast proliferation, down‑regulates transforming growth factor‑beta (TGF‑β), and limits oxidative stress. Clinical trials confirmed a ~50% reduction in the decline of forced vital capacity (FVC) over a year.
The Main Alternative: Nintedanib (Ofev)
Nintedanib (marketed as Ofev) is a tyrosine‑kinase inhibitor that blocks receptors involved in fibrotic signaling, such as PDGF, FGFR, and VEGFR. Like Esbriet, it was approved by the FDA in 2014 for IPF. Head‑to‑head data from the INJOURNEY study suggest similar efficacy in slowing FVC decline, but the safety and dosing experience differ markedly.
Key Differences in Mechanism of Action
- Esbriet (Pirfenidone): Primarily anti‑oxidant and anti‑inflammatory; targets TGF‑β signaling.
- Nintedanib (Ofev): Broad tyrosine‑kinase inhibition; blocks multiple growth factor pathways.
- Both drugs ultimately aim to reduce fibroblast activation, but the biochemical routes are distinct, which can influence side‑effect patterns and drug interactions.
Dosage and Administration
Esbriet is taken orally three times a day with meals. The titration schedule starts at 267 mg/day and climbs to the target 2403 mg/day over two weeks. Nintedanib is a twice‑daily capsule (150 mg each) taken with food, and the dose is fixed-no titration required.
Safety Profile and Common Side Effects
Understanding tolerability is crucial because both drugs are lifelong therapies.
| Drug | Most Frequent Side Effects | Serious Risks |
|---|---|---|
| Esbriet | GI upset (nausea, dyspepsia), skin rash, photosensitivity | Liver enzyme elevation (monitor ALT/AST), rare severe rash |
| Nintedanib | Diarrhea, abdominal pain, nausea | Elevated liver enzymes, increased bleeding risk (especially with anticoagulants) |
Both medications require baseline and periodic liver function tests. Esbriet’s photosensitivity means patients should avoid prolonged sun exposure and use SPF 30+ sunscreen daily.
Cost Considerations in Australia
Affordability often decides which drug a patient can sustain.
| Drug | Annual Cost (AU$) | Medicare/Pharmaceutical Benefits Scheme (PBS) Coverage |
|---|---|---|
| Esbriet | ~$34,000 | Partial PBS subsidy; out‑of‑pocket ~ $5,500 per year |
| Nintedanib | ~$38,000 | Similar PBS tier; out‑of‑pocket ~ $6,000 per year |
Prices fluctuate with generic entry, bulk purchasing, and state‑specific assist programs. Discuss with your pharmacist about compassionate use or manufacturer coupons.
Real‑World Patient Experiences
Clinical trial data are compelling, but everyday life adds nuance. A 2023 Australian registry tracked 214 IPF patients on either Esbriet or Nintedanib for two years. Findings:
- Adherence was higher with Esbriet (78%) than Nintedanib (68%) after the first six months, largely because GI side‑effects were more manageable with dose titration.
- Both groups showed a median 45% slower decline in FVC compared to historical controls.
- Healthcare utilization (hospital admissions for respiratory exacerbations) dropped by 30% in both cohorts.
These numbers suggest that while efficacy is parallel, the patient‑centered factors-like pill burden and side‑effect handling-can tip the balance.
When to Choose One Over the Other
Decision‑making should be individualized.
- Favor Esbriet if the patient has a history of severe diarrhea, is on anticoagulants, or prefers a thrice‑daily schedule that can be spread with meals.
- Favor Nintedanib for individuals who struggle with photosensitivity, have liver concerns that can be regularly monitored, or prefer a twice‑daily regimen.
- Consider combination therapy only within clinical trial settings; current guidelines advise against simultaneous use due to additive toxicity.
Always involve a pulmonologist, pharmacist, and, when possible, a patient support group to weigh these factors.
Future Directions and Emerging Alternatives
Research continues beyond the two approved drugs. Promising pipelines include:
- Pamrevlumab: An anti‑connective tissue growth factor (CTGF) antibody showing slowed FVC decline in Phase 2 trials.
- PRM-151: Recombinant human pentraxin‑2 targeting innate immune pathways.
- Gene‑editing approaches that aim to correct fibroproliferative signaling at the DNA level - still early‑stage.
These candidates may reshape the treatment landscape in the next decade, offering options for patients who cannot tolerate existing therapies.
Quick Checklist for Choosing a Therapy
- Confirm diagnosis of IPF via high‑resolution CT and multidisciplinary review.
- Check baseline liver enzymes, CBC, and creatinine.
- Discuss side‑effect profiles and lifestyle impact.
- Review PBS subsidy eligibility and out‑of‑pocket cost.
- Schedule follow‑up every 3‑6 months to assess FVC, tolerability, and adherence.
Can I switch from Esbriet to Nintedanib?
Yes, a switch is possible but should be done under specialist supervision. A wash‑out period of at least 48 hours is recommended to minimize overlapping toxicity, and liver function tests should be repeated before starting the new drug.
What if I develop severe photosensitivity on Esbriet?
Immediately reduce sun exposure, apply broad‑spectrum sunscreen, and wear protective clothing. If rash persists, the doctor may lower the dose or consider changing to Nintedanib.
Is there a generic version of Pirfenidone?
As of 2025, no generic Pirfenidone is approved in Australia. Patent protections still apply, but some overseas markets have lower‑priced versions pending local regulatory review.
How do I manage Nintedanib‑induced diarrhea?
Start with loperamide at the first sign of loose stools, stay hydrated, and consider a low‑fiber diet. If diarrhea persists beyond two weeks, the physician may reduce the dose to 100 mg twice daily.
Are there any diet restrictions while on these drugs?
No strict restrictions, but taking Esbriet with meals reduces GI upset, and high‑fat meals can increase Nintedanib absorption, potentially worsening side effects. A balanced diet with adequate protein supports overall lung health.





Ron Lanham
October 20, 2025 AT 17:50When it comes to managing idiopathic pulmonary fibrosis, the stakes are higher than a simple preference for one pill over another, and we must confront the moral imperative to choose wisely; the data presented about Esbriet versus its rivals is not just a chart, it is a testament to the lives hanging in the balance, and as a community we have a duty to scrutinize every claim, every side effect, and every cost figure with relentless rigor. The mechanisms of action described-TGF‑beta inhibition for Pirfenidone and tyrosine‑kinase blockade for Nintedanib-are not abstract biochemical footnotes; they dictate real‑world tolerability, adherence, and ultimately, survival. One cannot ignore the fact that Esbriet's dosing schedule, though three times a day, allows a titration that can ease gastrointestinal distress, a point that speaks volumes about patient‑centered care. Conversely, the fixed dosing of Nintedanib might appear convenient, yet its notorious diarrhoea profile has forced many patients to abandon therapy altogether, a tragic outcome that must be highlighted in any honest discussion. Moreover, the cost analysis for Australian patients underscores a systemic failure: even with PBS subsidies, out‑of‑pocket expenses remain prohibitive, and we cannot sit idly by while financial toxicity drives patients toward suboptimal adherence.
In the real‑world registry data, the higher adherence rate for Esbriet (78%) versus Nintedanib (68%) is not a trivial statistic; it reflects a complex interplay of side‑effect management, dosing flexibility, and patient education. The reduction in respiratory exacerbations by 30% across both cohorts should galvanize us to prioritize therapies that patients can sustain long term, rather than merely the ones that look good on paper. The safety profiles further reinforce this point: while both drugs demand regular liver function monitoring, the photosensitivity of Pirfenidone is a manageable risk with sunscreen, whereas the bleeding risk associated with Nintedanib, especially in patients on anticoagulants, is a grave concern that cannot be dismissed.
Ethically, we must also consider the future pipeline-Pamrevlumab, PRM‑151, and gene‑editing approaches-because abandoning current treatments in favor of speculative breakthroughs would betray the trust of those currently battling this relentless disease. The decision between Esbriet and its alternatives must be individualized, weighing comorbidities, lifestyle, and even geographic cost variables, but never should the choice be reduced to a headline slogan. In practice, clinicians should convene multidisciplinary teams, involve patient support groups, and document shared decision‑making processes, thereby honoring the autonomy and dignity of every individual facing IPF. Ultimately, the call to action is clear: we must champion evidence‑based, patient‑friendly, and economically viable options, and hold the healthcare system accountable for delivering them without compromise.
Deja Scott
October 20, 2025 AT 17:53The comparative overview does a solid job of laying out the key points without overwhelming the reader; the tables on side effects and cost in Australia are especially helpful for anyone trying to weigh practical considerations alongside clinical efficacy. I appreciate the emphasis on multidisciplinary involvement, which aligns with best practices in chronic disease management. The mention of emerging therapies provides a hopeful glimpse without overpromising. Overall, the guide is balanced and informative.
Natalie Morgan
October 20, 2025 AT 17:58Reading through the breakdown it becomes clear that both Esbriet and Nintedanib have their own sets of challenges but also distinct advantages especially when you look at how patients actually live with the drugs day to day
Mahesh Upadhyay
October 20, 2025 AT 18:03Only a fool would ignore the glaring evidence against Nintedanib!
Rajesh Myadam
October 20, 2025 AT 18:10I hear your frustration, and it’s understandable to feel uneasy about the side‑effect profile of any medication. While the concerns about Nintedanib’s diarrhea are valid, many clinicians have found success with dose adjustments and supportive care. It’s also worth noting that each patient’s tolerance can differ dramatically, so personal experience may vary. Ultimately, open dialogue with your healthcare team can help tailor the best approach for you.
Andrew Hernandez
October 20, 2025 AT 18:16The article’s side‑effect tables are a great quick reference especially for patients juggling daily schedules and trying to avoid unexpected costs.
Alex Pegg
October 20, 2025 AT 18:25While the data look balanced, the reality is that many patients are forced to choose based on availability rather than clinical superiority. The emphasis on subsidies glosses over the real financial strain. A truly impartial guide would highlight the hidden barriers more starkly.
laura wood
October 20, 2025 AT 18:33It’s encouraging to see a thorough comparison that doesn’t shy away from discussing both the pros and cons of each therapy. The practical tips on managing photosensitivity and diarrhea are especially useful for day‑to‑day living. I hope more clinicians share this kind of nuanced guidance with their patients.
Kate McKay
October 20, 2025 AT 18:43Absolutely, the actionable advice on side‑effect mitigation can really empower patients to stay on therapy longer. When you pair that with regular monitoring, you’re setting the stage for better outcomes. Keep spreading this kind of supportive information; it makes a tangible difference in people’s lives.
Demetri Huyler
October 20, 2025 AT 18:55Let’s be honest, the level of detail in this post is something most lay‑person articles lack, showing a depth that only true connoisseurs of medical literature can appreciate. It’s a reminder that not every source is created equal, and we should demand this caliber of insight from our healthcare conversations.
JessicaAnn Sutton
October 20, 2025 AT 19:08The exposition is meticulously structured, with each section logically progressing from pathophysiology to practical considerations, thereby facilitating a comprehensive understanding for readers. Moreover, the inclusion of both quantitative data and qualitative patient experiences enriches the narrative, offering a balanced perspective that is often absent in oversimplified summaries. The precision in language reflects a commendable commitment to accuracy, which is essential when discussing treatments that bear significant clinical weight. It would, however, be advantageous to integrate a brief discussion on the socioeconomic disparities that influence drug accessibility, as this factor undeniably shapes therapeutic decisions. Overall, the composition exemplifies scholarly rigor while remaining accessible to a broader audience.
Israel Emory
October 20, 2025 AT 19:23Indeed, the article does a remarkable job of weaving together clinical data, patient anecdotes, and cost analyses, providing a multifaceted view that is both informative and empathetic; however, it is essential to remember that individual experiences can vary widely, and ongoing dialogue with healthcare providers remains paramount, especially when navigating complex treatment landscapes; consequently, readers should feel encouraged to ask questions, seek second opinions, and stay informed about emerging therapies, all while balancing personal preferences and practical constraints.