Diabetes Eye Inflammation Risk Calculator
Your Eye Inflammation Risk Assessment
Key Takeaways
- High blood sugar can ignite inflammatory pathways in the eye, raising the risk of conditions like uveitis and diabetic retinopathy.
- Early signs include redness, pain, blurred vision, and floaters-don’t wait for vision loss to act.
- Strict glucose control, regular eye exams, and anti‑inflammatory diet habits cut the odds dramatically.
- Recognizing the link helps doctors treat eye inflammation faster and customize diabetes management.
When you hear the words Diabetes is a chronic condition where the body can’t regulate blood glucose effectively. Over time, the excess sugar damages tiny blood vessels and fuels chronic inflammation throughout the body.
Eye inflammation, medically termed ocular inflammation and often manifested as uveitis or conjunctivitis, is the eye’s response to infection, auto‑immunity, or irritants. In people with Diabetes, the inflammatory response is amplified, leading to a higher chance of serious eye problems.
Why High Blood Sugar Sparks Inflammation in the Eye
Three biological mechanisms tie elevated blood glucose to ocular inflammation:
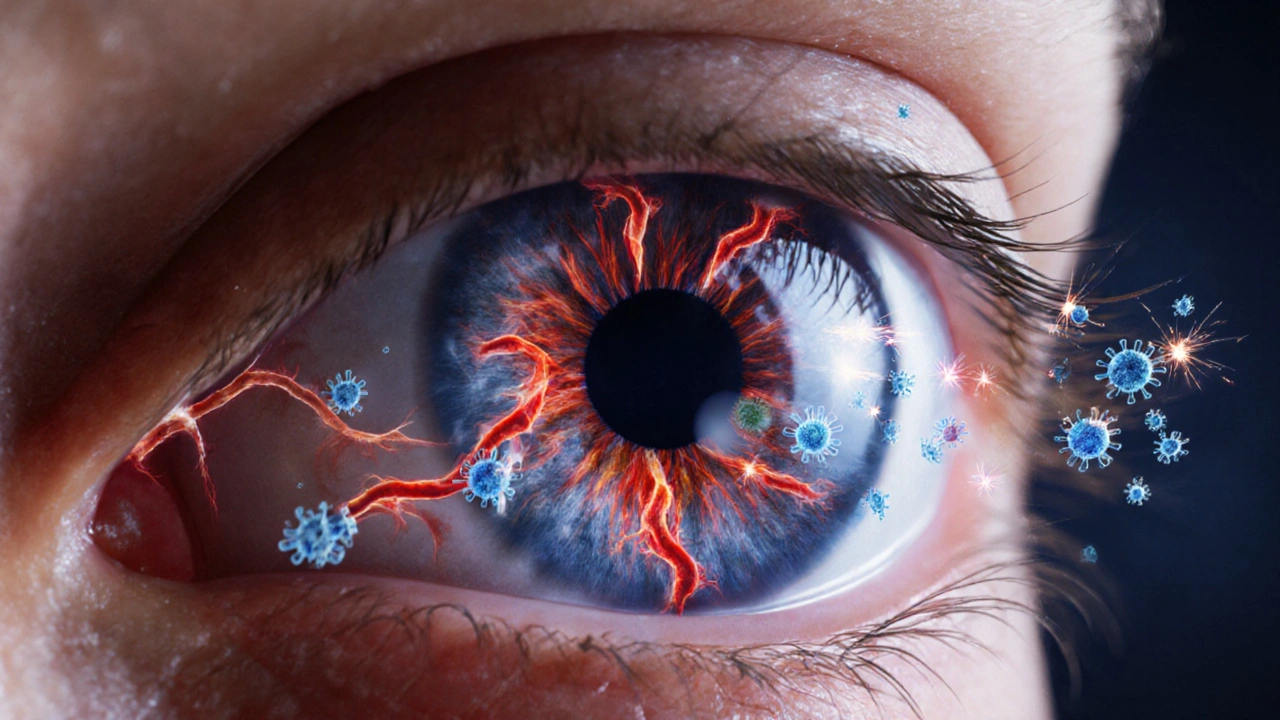
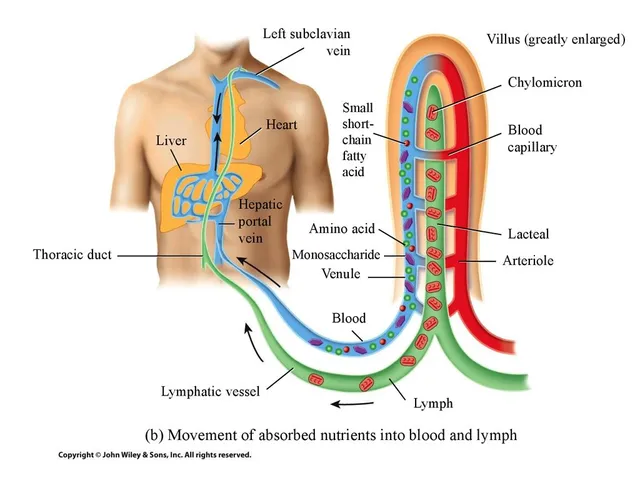
- Advanced Glycation End‑Products (AGEs): Excess glucose binds to proteins in the retina, forming AGEs. These sticky molecules attract immune cells and release cytokines such as interleukin‑6 (IL‑6) and tumor necrosis factor‑alpha (TNF‑α), which inflame vascular walls.
- Oxidative Stress: Hyperglycemia creates free radicals that damage the retina. Damaged cells send distress signals that further activate the immune system.
- Microvascular Leakage: Tight junctions between retinal capillaries weaken, allowing plasma proteins to seep into the eye’s interior and provoke inflammation.
These pathways don’t just stay in the retina; they affect the entire ocular structure, making conditions like uveitis more common among diabetics.

Common Eye Inflammation Conditions Linked to Diabetes
| Condition | Typical Symptoms | Prevalence in Diabetes | Prevalence in Non‑Diabetics |
|---|---|---|---|
| Uveitis | Redness, pain, photophobia, floaters | ~12% of diabetic patients | ~4% |
| Diabetic Retinopathy (inflamed stage) | Blurred vision, dark spots, occasional hemorrhage | 30‑40% of long‑term diabetics | Rare (≈1%) |
| Conjunctivitis (bacterial/viral) | Watery or purulent discharge, itching | ~18% | ~10% |
Spotting Early Warning Signs
Because inflammation can sneak in before you notice vision loss, watch for these cues:
- Persistent eye redness that doesn’t clear in a day or two.
- Sharp or dull ache around the eye, especially after meals high in sugar.
- Sudden increase in floaters or flashes of light.
- Blurry or double vision that fluctuates with blood‑sugar spikes.
- Dry or gritty feeling that feels unrelated to environmental factors.
If any of these pop up, schedule an eye exam within a week. Early detection can prevent permanent damage.
How to Reduce the Risk of Inflammation
Managing Diabetes and protecting your eyes go hand‑in‑hand. Here’s a practical checklist you can start today:
- Maintain Target Blood Glucose: Aim for fasting < 100mg/dL and post‑meal < 140mg/dL. Use continuous glucose monitors (CGM) to spot spikes.
- Regular Eye Exams: Every six months if you have Type1 or long‑standing Type2; annually if well‑controlled.
- Anti‑Inflammatory Diet: Load up on omega‑3 fatty acids (salmon, walnuts), leafy greens, and berries. Cut processed sugars and trans fats.
- Stay Active: Moderate exercise improves insulin sensitivity and reduces systemic inflammation.
- Medication Review: Some drugs (e.g., GLP‑1 agonists) have added anti‑inflammatory benefits. Discuss with your endocrinologist.
- Protect Your Eyes: Wear UV‑blocking sunglasses, avoid smoke‑filled rooms, and use lubricating drops if you’re prone to dryness.
Treatment Options When Inflammation Occurs
If you’re diagnosed with an inflammatory eye condition, treatment typically follows a tiered approach:
- Topical Steroids: Reduce local inflammation fast but require monitoring for increased eye pressure.
- Corticosteroid‑Sparing Agents: Drugs like methotrexate or biologics (e.g., adalimumab) target cytokine pathways without the side‑effects of steroids.
- Laser Therapy: For diabetic retinopathy, photocoagulation seals leaking vessels and curbs swelling.
- Intravitreal Injections: Anti‑VEGF agents (e.g., ranibizumab) block vascular growth factors that contribute to both neovascularisation and inflammation.
Co‑ordinating care between an ophthalmologist, endocrinologist, and primary care doctor ensures you’re tackling both the sugar level and the eye issue at the same time.
Living With Diabetes and Healthy Eyes: Real‑World Stories
Sarah, a 45‑year‑old teacher from Brisbane, thought she was fine after her Type2 diagnosis. Six months later, a sudden “red‑eye” episode left her struggling to read. An eye specialist discovered early‑stage uveitis linked to her fluctuating glucose. By tightening her CGM targets, adding omega‑3 supplements, and using a short course of topical steroids, Sarah’s vision returned and she’s now on a six‑month check‑in schedule.
Mark, a 62‑year‑old retiree, had well‑controlled diabetes but ignored yearly eye checks. He eventually developed proliferative diabetic retinopathy, requiring laser surgery and multiple anti‑VEGF injections. Mark’s story highlights that even perfect glucose numbers can’t replace regular eye screenings.
Frequently Asked Questions
Can high blood sugar cause eye redness?
Yes. Elevated glucose triggers inflammatory cytokines that can irritate the conjunctiva, leading to persistent redness.
Is uveitis more common in Type1 or Type2 diabetes?
Studies show a slightly higher incidence in Type1, likely because autoimmune factors overlap, but both types carry a notably increased risk compared to non‑diabetics.
Do anti‑diabetic medications reduce eye inflammation?
Some newer agents, especially GLP‑1 receptor agonists, have shown modest anti‑inflammatory effects in retinal tissue, but they are not a substitute for dedicated eye treatments.
How often should a diabetic get an eye exam?
At least once a year, though many specialists recommend a six‑month schedule if you have any signs of retinopathy or a history of ocular inflammation.
Can lifestyle changes reverse eye inflammation?
Early‑stage inflammation often improves with tighter glucose control, anti‑inflammatory diet, and regular exercise. Advanced cases may still need medical therapy.
Understanding the link between Diabetes and eye inflammation empowers you to act before vision loss sets in. Keep your blood sugar steady, stay on top of eye exams, and don’t ignore a red or painful eye-your sight depends on it.
14 Comments
Write a comment
RELATED POSTS





Geneva Lyra
October 7, 2025 AT 13:30Great breakdown of how high glucose can light up the inflammatory pathways in the eye. I totally agree that keeping a close eye on those HbA1c numbers can save a lot of headache later. Also, the tip about omega‑3s is super useful – I’ve started adding walnuts to my morning oatmeal and feel better already!
Moritz Bender
October 17, 2025 AT 23:30From a clinical perspective, the mechanistic cascade you outlined aligns well with the current literature on advanced glycation end‑products (AGEs) and oxidative stress. The interplay between IL‑6, TNF‑α and microvascular leakage is a classic example of hyperglycemic‑induced cytokine storm within the retinal milieu. 📊
Implementing CGM data to modulate insulin dosing could directly attenuate AGE formation, thereby reducing the propensity for uveitic flare‑ups. Moreover, the recommendation to incorporate GLP‑1 receptor agonists is on point; emerging trials demonstrate a modest reduction in retinal edema incidence. Overall, your risk calculator is a pragmatic tool for both endocrinologists and ophthalmologists.
Nicole Hernandez
October 28, 2025 AT 08:30Thank you for the thorough overview. The distinction between Type 1 and Type 2 incidence rates of uveitis is particularly helpful for patient counseling. Emphasizing regular six‑month eye exams for long‑standing diabetics is a sensible preventive measure. I also appreciate the clear dietary suggestions; increasing omega‑3 intake can indeed modulate systemic inflammation. Looking forward to seeing more data on the anti‑inflammatory benefits of newer antidiabetic agents.
florence tobiag
November 7, 2025 AT 18:30Hold up-are we really supposed to trust a calculator that was apparently cobbled together by a web‑designer with no medical credentials?!? The whole "average HbA1c" metric is oversimplified; you can't reduce a complex immunological response to a single percentage value!!! Also, the suggestion that "once a year" exams are enough for **all** diabetics is dangerously misleading-people with the longest disease duration need quarterly checks!!!
Don't let the glossy UI distract you from the fact that this is just a gimmick!!!
Terry Washington
November 18, 2025 AT 04:30The drama of eye inflammation is no joke – the sight‑stealing intruder that creeps in while you ignore the sugar spikes! The stakes are high, and only swift, decisive action (think aggressive steroid‑sparing protocols) will keep your vision intact. Don’t be complacent; confront the fire before it devours your retina!
Claire Smith
November 28, 2025 AT 14:30This article is concise and useful.
Émilie Maurice
December 9, 2025 AT 00:30While the piece is generally accurate, it neglects to mention the importance of consistent blood pressure control, which is a critical factor in retinal health.
Ellie Haynal
December 19, 2025 AT 10:30I love how the article balances medical detail with actionable steps. The checklist format makes it easy to share with friends who are newly diagnosed. Also, the real‑world stories of Sarah and Mark illustrate that lifestyle tweaks can truly shift outcomes.
Jimmy Gammell
December 29, 2025 AT 20:30Solid info! 👍 Remember, consistency is key: keep your CGM alerts on, hit those exercise days, and don’t skip the eye appointments. You’ve got this!
fred warner
January 9, 2026 AT 06:30Excellent guide! The energy you bring to the topic really motivates me to stay on top of my eye health.
Veronica Mayfair
January 19, 2026 AT 16:30👍💡 This is super helpful! Keep the tips coming! 😊
Rahul Kr
January 30, 2026 AT 02:30Interesting read. The clinical details are spot‑on, and the preventive checklist is practical for daily routine.
Anthony Coppedge
February 9, 2026 AT 12:30Reading through the mechanisms of diabetic ocular inflammation reminded me of the intricate feedback loops described in immunology textbooks. First, the formation of advanced glycation end‑products (AGEs) creates a reservoir of neo‑antigens that the innate immune system cannot ignore. Second, those AGEs bind to RAGE receptors on retinal endothelial cells, initiating a cascade that up‑regulates NF‑κB transcription factors. Third, the NF‑κB activation leads to the production of pro‑inflammatory cytokines such as IL‑6, IL‑1β, and tumor necrosis factor‑alpha. Fourth, these cytokines increase vascular permeability, allowing plasma proteins to leak into the retinal extracellular space. Fifth, the resultant edema further compromises photoreceptor function, creating a feedback loop of hypoxia and inflammation. Sixth, oxidative stress from hyperglycemia generates reactive oxygen species, which damage mitochondrial DNA in retinal cells. Seventh, mitochondrial dysfunction amplifies the production of inflammatory mediators, exacerbating cellular injury. Eighth, microvascular leakage facilitates the recruitment of leukocytes, which release proteolytic enzymes that degrade the basement membrane. Ninth, this degradation compromises the blood‑retinal barrier, making the eye more susceptible to infection and further inflammation. Tenth, chronic inflammation can trigger neovascularization, a hallmark of proliferative diabetic retinopathy. Eleventh, anti‑VEGF therapy, while effective at reducing neovascular growth, does not address the upstream inflammatory triggers. Twelfth, lifestyle interventions such as a Mediterranean‑type diet rich in omega‑3 fatty acids can modulate the inflammatory milieu by reducing arachidonic acid‑derived eicosanoids. Thirteenth, regular aerobic exercise improves insulin sensitivity, thereby lowering systemic glucose levels and reducing AGE formation. Fourteenth, consistent use of anti‑inflammatory agents like low‑dose aspirin may provide adjunctive protection by inhibiting platelet aggregation and subsequent micro‑thrombi formation in retinal vessels. Fifteenth, in clinical practice, a multi‑disciplinary approach involving endocrinologists, ophthalmologists, and nutritionists yields the best outcomes for patients. In summary, the interplay of metabolic, vascular, and immunologic factors creates a perfect storm for ocular inflammation in diabetes, and comprehensive management must address each component.
Joshua Logronio
February 19, 2026 AT 22:30Just a heads‑up: some of those “new” anti‑inflammatory meds might be part of a larger pharma push to get us all hooked on more prescriptions. Keep an eye on the fine print.