Dizziness Type Identifier
Select Your Symptoms
Choose all that apply to describe your dizziness experience:
Identify Triggers
Which situations commonly bring on your dizziness?
Your Dizziness Type Analysis
Ever felt the room spin for a second and then wondered why it seemed harder to stay steady? That uneasy feeling isn’t just a random glitch - it’s often a signal that your balance system and your sense of dizziness are talking to each other. In this article we’ll untangle what dizziness really is, how it ties into balance problems, and what you can do the next time the world tilts.
What dizziness actually means
Dizziness is a catch‑all term for a range of sensations that make you feel off‑balance, light‑headed, or like the room is moving. Some people describe it as "the room is spinning" (that's vertigo), others say they feel about to faint (presyncope), and some just feel unsteady on their feet (disequilibrium). The key is that dizziness is a symptom, not a disease by itself.
Defining balance disorders
Balance disorders are conditions that impair the body’s ability to maintain a stable position, whether you’re standing still or moving. They can stem from problems in the inner ear, the brain, muscles, or even the eyes. When something goes wrong, you might sway, stumble, or have a hard time walking straight.
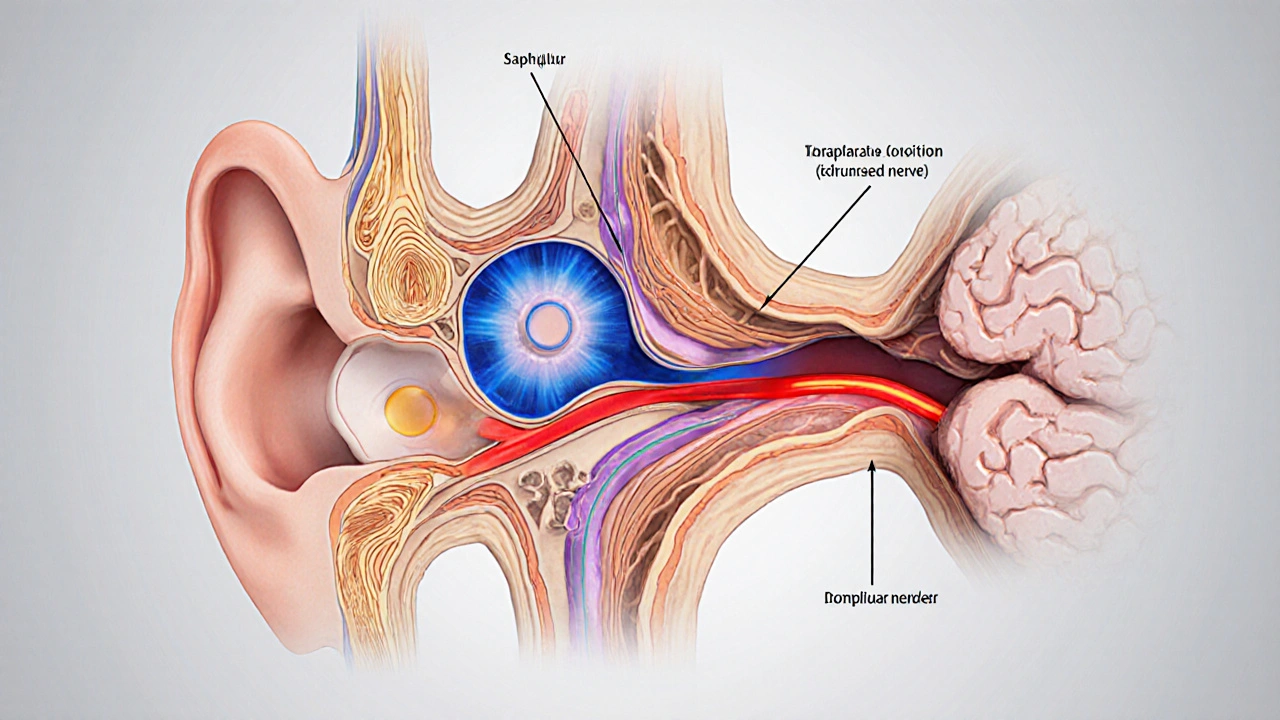
The vestibular system - the bridge between dizziness and balance
Think of the vestibular system as the body’s built‑in gyroscope. It lives in the inner ear and talks to the brain about head motion and position. The system has three parts:
- Semicircular canals - detect rotation.
- Otolith organs - sense linear acceleration and gravity.
- Vestibular nerve - carries the signal to the brainstem and cerebellum.
Inner ear houses these canals and otolith organs, and any fluid or structural disturbance there can trigger both dizziness and a loss of balance.
Common conditions that cause both dizziness and balance problems
Below are the usual suspects that make the two symptoms appear together.
- Benign paroxysmal positional vertigo (BPPV) occurs when tiny calcium crystals shift into the semicircular canals, causing brief, intense spinning when you tilt your head.
- Meniere’s disease is an inner‑ear disorder marked by fluctuating hearing loss, ringing in the ears, and episodes of vertigo that can last hours.
- Vestibular migraine produces vertigo or a sense of disequilibrium that may last minutes to days, often alongside a headache.
- Stroke or transient ischemic attack (TIA) in the cerebellum or brainstem can suddenly disrupt vestibular signaling, leading to severe dizziness and inability to coordinate movements.
- Orthostatic hypotension drops blood pressure when you stand up too fast, causing light‑headedness and a wobble as the brain momentarily loses blood flow.
- Side‑effects from certain medications (e.g., antihistamines, blood pressure meds, sedatives) can blunt vestibular function or alter blood pressure, producing both sensations.
Quick self‑check: what kind of dizziness are you feeling?
| Type | Typical sensation | Common triggers | What to watch for |
|---|---|---|---|
| Vertigo | Spinning or a feeling that surroundings are moving | Head position change, inner‑ear problems | Falls, nausea, lasting seconds to hours |
| Presyncope | Light‑headed, like you might faint | Sudden standing, dehydration, low blood pressure | Blurred vision, sweating, fainting risk |
| Disequilibrium | Unsteady, like you can’t keep your balance | Neurological disease, vision loss, muscle weakness | Tripping, difficulty walking straight |
If the episode feels more like a brief spin after you lie down, BPPV is likely. Light‑headedness after a quick stand points toward orthostatic hypotension. A constant wobble that worsens with multitasking could hint at a neurological cause.
When should you see a professional?
Even though many dizziness spells resolve on their own, you’d want a clinician if you notice any of these red flags:
- Sudden, severe vertigo that follows a head injury.
- New neurological signs - double vision, slurred speech, weakness.
- Persistent dizziness lasting more than a week.
- Fainting episodes or blackouts.
- Associated chest pain, shortness of breath, or severe headache.
Primary care doctors, ENT specialists, and neurologists can run tests like the Dix‑Hallpike maneuver for BPPV, audiograms for Meniere’s, or MRI scans for central causes.

Basic management strategies you can start today
Here are some practical steps that work for many patients:
- Repositioning maneuvers - For BPPV, the Epley or Semont moves can reset displaced crystals. You can learn them from a therapist or reputable video guides.
- Hydration & salt balance - Low blood volume fuels orthostatic drops. Drink enough water and consider a pinch of salt if you’re not on a low‑sodium diet.
- Vestibular rehab exercises - Simple head‑turn and gaze‑stabilization drills improve the brain’s ability to compensate for inner‑ear deficits.
- Medication review - Ask your doctor if any current prescriptions could be contributing to dizziness and whether alternatives exist.
- Stress & migraine control - For vestibular migraine, tracking triggers (caffeine, bright lights) and using prescribed migraine prophylaxis can cut vertigo episodes.
- Balance training - Standing on one foot, heel‑to‑toe walks, or using a balance board reduces fall risk, especially in older adults.
Always start any new exercise under professional guidance if you’re unsure about safety.
Key takeaways checklist
- Identify the type of dizziness - vertigo, presyncope, or disequilibrium.
- Notice triggers: head position, standing quickly, medication changes.
- Watch for red‑flag symptoms that need urgent care.
- Consider simple home maneuvers (Epley) for BPPV.
- Stay hydrated, review meds, and practice balance exercises.
Frequently Asked Questions
Why does my dizziness feel different when I lie down versus when I stand up?
Changing positions alters the fluid movement in the inner ear. Lying down can trigger BPPV‑related spinning, while standing up quickly can cause a drop in blood pressure, leading to light‑headedness. The underlying mechanism is distinct, which is why the sensation changes.
Can anxiety cause dizziness and balance problems?
Yes. Panic attacks can hyperventilate you, lowering CO₂ levels and making you feel faint or unsteady. Anxiety also tightens neck muscles, which can affect proprioceptive input, subtly shaking your balance.
Is it safe to do the Epley maneuver at home?
For most adults with classic BPPV, the Epley can be safely performed alone after a brief instruction from a clinician. If you feel nausea, vomiting, or if symptoms don’t improve after a few tries, seek professional help.
What lifestyle changes help prevent dizziness?
Stay hydrated, rise slowly from sitting or lying, keep a regular sleep schedule, limit alcohol, and maintain a balanced diet rich in potassium and magnesium. Regular low‑impact cardio improves circulation, reducing orthostatic episodes.
When is dizziness a sign of something serious like a stroke?
If dizziness comes with sudden severe headache, facial droop, slurred speech, loss of vision, or weakness on one side, treat it as a possible stroke and call emergency services immediately. These symptoms indicate brain involvement beyond the inner ear.






Lindy Swanson
October 8, 2025 AT 20:23Sure, dizziness is just a minor inconvenience, nothing worth the hype.
Amit Kumar
October 9, 2025 AT 01:56Hey folks! 😊 This article breaks it down nicely. I love how it ties vertigo to inner‑ear issues and gives simple home tricks like the Epley. Definitely useful for anyone feeling like the world’s spinning.
Crystal Heim
October 9, 2025 AT 07:30Honestly the piece is a rehash of basic ENT textbook content. No new insights here.
Calvin Smith
October 9, 2025 AT 13:03Oh wow, Crystal, way to state the obvious with all the enthusiasm of a snail on a treadmill. 🙄 If you wanted a fresh take, maybe add something about vestibular rehab instead of just calling it a “textbook.”
Brenda Hampton
October 9, 2025 AT 18:36Calvin, I get your sarcasm but let’s keep it constructive. The article actually does a good job summarizing the basics for newcomers, and the Epley instructions are a solid practical tip.
Lara A.
October 10, 2025 AT 00:10Everyone’s ignoring the real cause-governmental labs are testing frequency‑based mind‑control through vestibular stimulation!!! Wake up!!!
Ashishkumar Jain
October 10, 2025 AT 05:43lol Lara, you're over the top as usual-no secret labs, just good old ear fluid. Stay chill, no need to hype it up.
Julie Sook-Man Chan
October 10, 2025 AT 11:16I appreciate the balanced tone of the article. It’s straightforward without being too clinical.
Danielle Ryan
October 10, 2025 AT 16:50Julie, seriously?? This post is sooo helpful!!! I’m practically vibrating with excitement!!! 😱💥
Deb Kovach
October 10, 2025 AT 22:23Great summary! 👍 The vestibular system is indeed the body’s built‑in gyroscope, and understanding that connection helps demystify those dizzy spells. I especially like the clear distinction between vertigo, presyncope, and disequilibrium-it makes self‑assessment easier. The table is a handy quick‑reference for anyone unsure which type they’re experiencing. You’ll notice that many triggers overlap, like rapid postural changes causing both BPPV‑related vertigo and orthostatic hypotension‑related light‑headedness. That’s why the article’s advice to stay hydrated and rise slowly is so practical. Also, the step‑by‑step Epley maneuver description is a lifesaver for BPPV sufferers; I’ve tried it myself and felt relief within minutes. For those with vestibular migraine, the tip to track caffeine, bright lights, and stress is on point-migraine diaries can reveal patterns. The emphasis on red‑flag symptoms, such as sudden severe headache or neurological deficits, is crucial; those warrant immediate medical attention. I’d add that regular balance training, like the heel‑to‑toe walk, can improve proprioception and reduce fall risk, especially in older adults. The article’s suggestion to review medications is spot‑on-many antihistamines and blood pressure drugs can worsen dizziness. One more thing: consider a low‑salt diet if you have Meniere’s disease; it can help control fluid buildup in the inner ear. Finally, the FAQ section addresses common concerns succinctly, and the use of emojis makes the content feel more approachable. Overall, a thorough, user‑friendly guide that balances medical detail with actionable tips. 👏😊
Sarah Pearce
October 11, 2025 AT 03:56Deb, nice work but the article could use more citations. Just saying.
Ajay Kumar
October 11, 2025 AT 09:30This piece really helped me understand why I feel off‑balance after standing up too fast. The advice to sip water and move slowly is something I’ll definitely try.
Richa Ajrekar
October 11, 2025 AT 15:03Ajay, your comment contains multiple grammatical errors and colloquial misspellings that undermine credibility. Please adhere to standard English conventions.
Pramod Hingmang
October 11, 2025 AT 20:36The article’s blend of medical facts and practical tips is spot‑on. I especially appreciate the colorful description of the vestibular system as a “gyroscope.”
Benjamin Hamel
October 12, 2025 AT 02:10While I respect the effort, I can’t help but notice the article skirts around the deeper complexities of central vertigo. It mentions strokes in passing but fails to explore how cerebellar lesions produce persistent disequilibrium distinct from peripheral causes. Moreover, the discussion on vestibular migraine barely scratches the surface, omitting the role of cortical spreading depression and its impact on vestibular nuclei. A truly comprehensive guide should also address the limitations of bedside tests like the Dix‑Hallpike in differentiating central versus peripheral pathology. Finally, the recommendation to “consult a healthcare professional” is vague; specifying when to seek an ENT versus a neurologist would be more actionable. In short, the piece is a good entry‑level overview but leaves out the nuanced diagnostic pathways that seasoned clinicians rely on.
Christian James Wood
October 12, 2025 AT 07:43Benjamin, you’re right to point out the gaps, but let’s not forget the article’s primary audience is laypeople looking for immediate relief. While your critique is academically sound, it risks alienating readers who simply need to know they should stay hydrated, rise slowly, and maybe try the Epley maneuver. Throwing in jargon about cortical spreading depression and cerebellar lesions without lay explanations could overwhelm the very people the guide aims to help. That said, a brief sidebar on when to suspect a central cause-like sudden onset of double vision or unilateral weakness-could bridge that gap nicely. Balancing depth with accessibility is the key. So, kudos for the thoroughness, but keep the tone user‑friendly.