Parkinson's Speech Symptom Checker
Symptom Assessment Tool
Answer the following questions about speech patterns to identify potential Parkinson's-related speech symptoms.
Assessment Results
Quick Takeaways
- Parkinson's disease often leads to Parkinson's disease speech changes such as soft voice, slurred articulation, and monotone pitch.
- Symptoms stem from dopamine loss, muscle rigidity, and impaired breath control.
- Early detection and regular monitoring can slow functional decline.
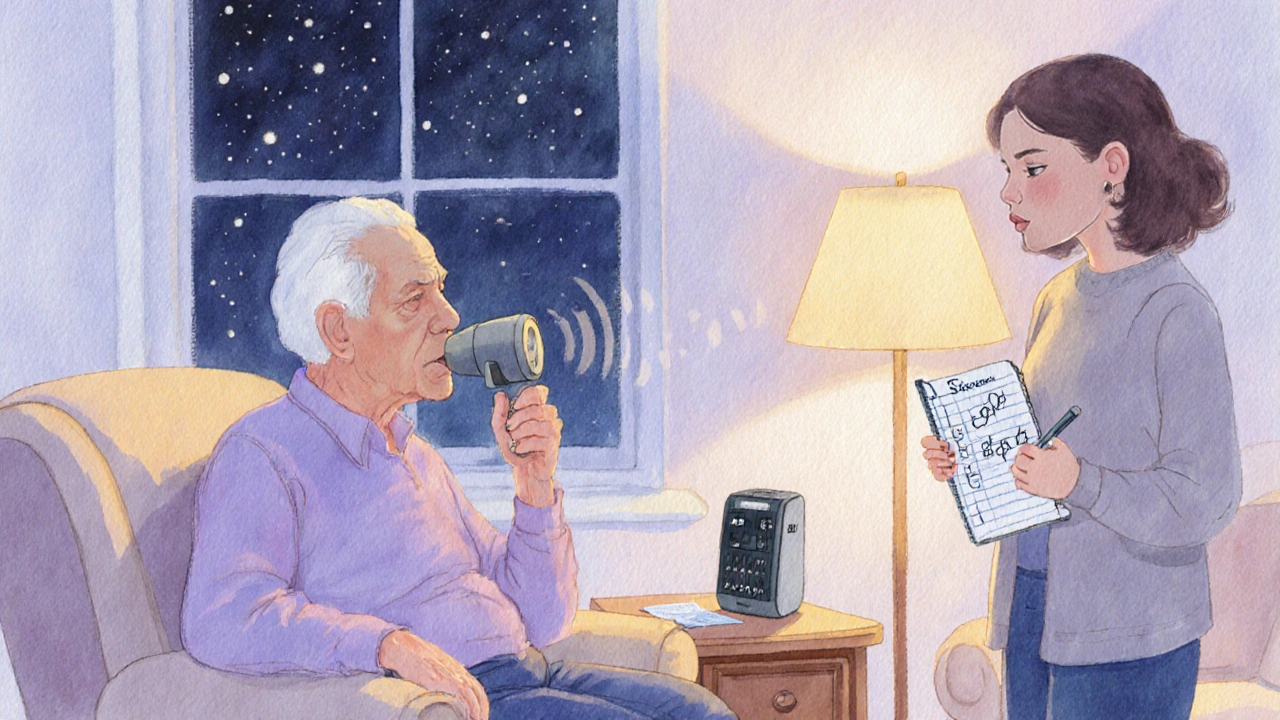
- Speech‑language pathology, voice‑amplification devices, and medication adjustments are the core management tools.
- Family members and caregivers play a crucial role in practicing exercises and creating supportive communication environments.
What Exactly Changes in Speech?
When doctors talk about Parkinson's disease is a progressive neurodegenerative disorder that primarily affects movement control, they often focus on tremor, stiffness, and slowness. Yet the voice is one of the first systems to show trouble. The most common pattern is called dysarthria is a motor speech disorder caused by weakened or uncoordinated muscles used for speech. In Parkinson’s, dysarthria usually presents as a “hypokinetic” type-soft, breathy, and rushed.
Other speech‑related issues include:
- Hypophonia is reduced vocal loudness that makes the speaker sound whisper‑like.
- Monotone pitch is loss of natural intonation, causing speech to sound flat.
- Articulation imprecision is slurred or unclear consonant production.
- Rapid rate is speaking too quickly, often called festinating speech.
Why Do These Changes Happen?
The root cause is the loss of dopamine‑producing neurons in the substantia nigra is a brain region that regulates movement and muscle tone. Dopamine helps fine‑tune the basal ganglia circuitry that coordinates breathing, vocal fold vibration, and facial muscle movement. When dopamine drops, the system becomes stiff and slow. This leads to:
- Reduced respiratory support for speech (weak breath pressure).
- Impaired coordination between the larynx and articulators (tongue, lips).
- Difficulty adjusting pitch and volume on the fly.
Medication such as levodopa is the primary drug that replenishes brain dopamine and improves motor function can help, but its effect on speech is variable. Some patients notice a modest boost in loudness, while others need additional therapy.

How to Spot Early Warning Signs
Because speech changes often precede noticeable gait problems, families should listen for these red flags during casual conversation:
- The person asks you to repeat themselves more than usual.
- They seem to be shouting without realizing it.
- Their sentences sound rushed or clipped.
- Emotional expression feels muted-no rise and fall in tone.
Documenting these observations in a simple log (date, situation, symptom) can help clinicians quantify progression and tailor interventions.
Therapeutic Options that Really Work
There are three proven pillars for managing speech issues in Parkinson’s:
| Approach | Key Technique | Typical Session Frequency | Evidence of Effectiveness |
|---|---|---|---|
| Loud‑Voice (Lee Silverman) Therapy | Intensive volume training; “think loud, speak loud” | 2-3 times/week, 45min each | Randomized trials show 10‑15dB increase in vocal intensity after 4weeks |
| Articulation‑Precision Exercises | Slow, exaggerated consonant drills (e.g., “p‑t‑k” sequences) | Daily home practice, 10min + weekly clinician visit | Improves intelligibility scores by 15‑20% in 6weeks |
| Respiratory‑Support Training | Breath‑holding and sustained phonation tasks | 3 sessions/month, integrated with other therapy | Boosts speech rate control and reduces choking episodes |
All three methods are typically delivered by a certified speech‑language pathologist is a health professional specialized in assessing and treating communication disorders. A therapist can also prescribe a portable voice‑amplification device for noisy environments.
Practical Tips You Can Use Today
Even without a therapist, simple habits make a noticeable difference:
- Use the “C-A-P” rule: Charge your voice, Articulate clearly, Pace slowly. Imagine you’re speaking to someone with hearing loss.
- Practice “speech breathing”: inhale through the nose for 2seconds, exhale while saying a sustained vowel (e.g., “ah”) for as long as possible.
- Record a 30‑second story, then play it back. Notice volume, speed, and clarity; adjust on the next try.
- Reduce background noise at home - turn off the TV while chatting, sit facing the speaker, and use a small tabletop microphone if needed.
- Encourage family members to ask “Can you repeat that?” only when truly needed; constant prompting can increase anxiety and worsen voice strain.
When to Call a Professional
If any of the following occur, schedule a consultation with a speech‑language pathologist promptly:
- Intelligibility drops below 80% in everyday conversations.
- Voice fatigue after speaking for less than 5minutes.
- Frequent misunderstandings leading to safety risks (e.g., missed medication instructions).
- Significant emotional distress linked to communication difficulties.
Early referral often means fewer sessions are needed to reclaim functional speech.
Frequently Asked Questions
Does medication improve speech in Parkinson’s?
Levodopa can raise overall motor tone, which sometimes boosts loudness, but it rarely fixes articulation or pitch variation. Combining meds with targeted speech therapy gives the best results.
Can deep‑brain stimulation (DBS) help voice problems?
DBS of the subthalamic nucleus often improves gait and tremor, yet its impact on speech is mixed. Some patients experience clearer speech; others notice new dysarthria. A thorough pre‑op speech evaluation is essential.
Is there a cure for Parkinson’s‑related speech loss?
No cure exists yet. However, consistent therapy can maintain or even improve communication ability for many years.
How long does Lee Silverman Voice Treatment (LSVT) last?
A standard LSVT‑LOUD program runs for 4weeks with 4 sessions per week. Maintenance boosters (1‑2 sessions per month) are often recommended after the intensive phase.
What home exercises work best for breath support?
Try the “in‑hale‑hold‑exhale” drill: inhale for 2seconds, hold for 1second, then exhale while counting aloud to 5. Repeat 5times, three times a day.
Putting It All Together
Speech and communication are core to identity. When Parkinson’s disease threatens these skills, early awareness, regular monitoring, and a multi‑modal treatment plan can preserve quality of life. Empower yourself or your loved one by tracking changes, practicing daily exercises, and seeking professional help before frustration turns into isolation.





cris wasala
October 5, 2025 AT 17:58Great rundown, thanks!
Tyler Johnson
October 8, 2025 AT 01:32I’ve seen a lot of patients where the first thing they notice is that they have to ask people to repeat themselves over and over. It’s like the brain’s volume knob is stuck on low and the rest of the body is still trying to keep up. The article nails the fact that hypophonia often shows up before tremor gets bad enough to notice. Also, the C‑A‑P rule is a solid, practical tool you can start using today. Keep spreading the word – early awareness makes a huge difference.
Annie Thompson
October 10, 2025 AT 09:05Reading through this piece reminded me of the first time my dad started whispering during family gatherings – nobody realized it was a symptom until the doctor mentioned hypokinetic dysarthria. The way Parkinson’s steals the natural melody of speech is both heartbreaking and fascinating; it’s as if the brain’s orchestra lost its conductor, leaving the instruments playing flat and out of sync. One of the earliest clues is the sudden need to ask, “Can you say that again?” because the volume drops without the speaker even noticing. That loss of vocal intensity, known as hypophonia, can be measured in decibels, and a 10‑15 dB boost after a short LSVT‑LOUD program is nothing short of miraculous for many. But volume is just one piece of the puzzle; the monotone pitch that follows makes even the most expressive person sound robotic, stripping away emotional nuance from everyday conversation. Articulation imprecision creeps in as well, with consonants becoming fuzzy, turning “talk” into “tawk” and making it harder for listeners to understand. When speech speed spikes into a rapid, clipped cadence – the so‑called festinating speech – it’s a clear sign that the basal ganglia’s timing circuitry is faltering. The article correctly points out that dopamine loss in the substantia nigra is the root cause, but it’s the downstream effects on respiratory support and laryngeal coordination that really manifest as speech changes. Levodopa can lift the overall motor tone, sometimes giving a modest lift to loudness, yet it rarely smooths out the articulation or restores pitch variability on its own. That’s why a multidisciplinary approach, combining medication with targeted voice therapy, yields the best outcomes. The “C‑A‑P” rule – Charge your voice, Articulate clearly, Pace slowly – is a practical mantra that families can adopt without a therapist present. Recording yourself and listening back is a cheap yet powerful feedback loop to track progress over weeks. Reducing background noise, facing the speaker, and even using a small tabletop microphone can dramatically improve intelligibility in everyday settings. Moreover, involving caregivers in daily practice turns therapy into a shared activity, reinforcing both the patient’s confidence and the bond with loved ones. Finally, the article’s emphasis on early referral is spot‑on; catching these subtle changes before they cascade into severe communication breakdown can preserve quality of life for years.
Parth Gohil
October 12, 2025 AT 16:38From a clinician’s perspective, the jargon‑heavy section about basal‑ganglia circuitry is spot on, but you can simplify it for patients by saying the brain’s “speech engine” is losing fuel. In practice, we use the term "hypokinetic dysarthria" to bundle the soft voice, flat intonation, and rapid rate into one diagnostic bucket. The table you included is a nice quick‑look for therapists to pick the right protocol – LSVT‑LOUD for volume, articulation drills for clarity, and respiratory support for stamina. I’d add that a portable voice‑amplifier can be a game‑changer in noisy restaurants, letting the patient stay socially active without straining. Also, keep an eye on medication timing; sometimes taking levodopa right before a therapy session spikes vocal output temporarily. All in all, the article packs a lot of actionable advice for both clinicians and families.
VAISHAKH Chandran
October 15, 2025 AT 00:12Interesting read, though I think the hype around LSVT is a bit overblown – not every patient needs an elite program.
Pat Merrill
October 17, 2025 AT 07:45Sure, “early detection” sounds noble until you realize most people ignore the subtle voice clues until it’s too late – typical medical optimism.
Ian Parkin
October 19, 2025 AT 15:18I concur with the earlier points, particularly the emphasis on structured therapy. The evidence base for LSVT‑LOUD, though not flawless, does show statistically significant gains in vocal intensity after four weeks of intensive training. Moreover, integrating articulation drills alongside volume work ensures comprehensive improvement, rather than focusing on a single dimension of speech. It is vital for clinicians to tailor the program to each patient’s specific deficits, as a one‑size‑fits‑all approach can lead to suboptimal outcomes. In summary, a multimodal regimen, as outlined, remains the gold standard.
Howard Mcintosh
October 21, 2025 AT 22:52Anyone can try the "speech breathing" drill at home – inhale for two seconds, then exhale on a sustained "ah" as long as possible. It’s a quick way to boost breath support before a phone call.
Jeremy Laporte
October 24, 2025 AT 06:25Totally agree, that simple drill can make a huge difference, especially when you practice it daily with a friend for accountability.
Anthony MEMENTO
October 26, 2025 AT 12:58Let’s not forget that medication timing can masquerade as therapy gains; a dopamine boost right before a session can inflate the perceived benefit of any voice exercise.
aishwarya venu
October 28, 2025 AT 20:32Exactly, and that’s why tracking medication schedules alongside speech logs is crucial – otherwise you might attribute a temporary lift to the wrong intervention.
Nicole Koshen
October 31, 2025 AT 04:05Deep‑brain stimulation (DBS) often helps gait but its impact on speech is mixed; some patients report clearer speech, others get a new layer of dysarthria.
Ed Norton
November 2, 2025 AT 11:38True, the pre‑op speech evaluation is essential to weigh the risks – you don’t want to trade better walking for worse communication.
Karen Misakyan
November 4, 2025 AT 19:12From a philosophical standpoint, the loss of vocal nuance can feel like losing a part of one’s identity; preserving speech is thus as much an existential pursuit as a medical one.
Amy Robbins
November 7, 2025 AT 02:45Well‑said, though the article could have mentioned how socioeconomic factors limit access to pricey voice‑amplifiers and intensive therapy – not everyone can afford the “gold standard.”
Michelle Zhao
November 9, 2025 AT 10:18All things considered, the key takeaway is that speech is a living, breathing reflection of our brain’s health, and caring for it early can keep the conversation going for years to come.