Hyponatremia Risk Calculator for Older Adults
Personal Risk Assessment
Symptom Checker
Risk Assessment Results
When you start an SSRI for depression, you expect to feel better-less sadness, more energy, clearer thinking. But for some people, especially older adults, the medication can trigger something far more dangerous: dangerously low sodium in the blood. This isn’t a rare glitch. It’s a well-documented, often missed side effect that can lead to confusion, falls, seizures, and even coma. And it happens faster than most doctors expect.
What Is Hyponatremia, and Why Does It Happen with SSRIs?
Hyponatremia means your blood sodium level drops below 135 mmol/L. Sodium is essential. It helps control fluid balance, nerve signals, and muscle function. When sodium gets too low, water floods into your cells-including brain cells. That’s when confusion, headaches, nausea, and dizziness start. In severe cases, below 125 mmol/L, seizures or coma can occur.
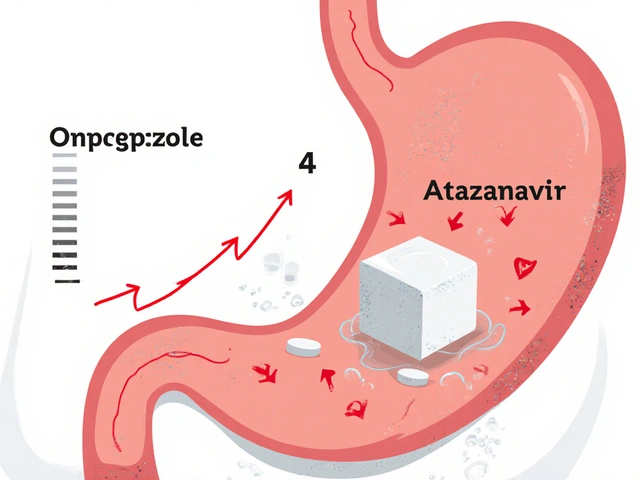
SSRIs like citalopram, sertraline, fluoxetine, and paroxetine cause this by overstimulating serotonin receptors in the brain. This tricks the body into releasing too much antidiuretic hormone (ADH). ADH tells your kidneys to hold onto water instead of flushing it out. More water in your blood means sodium gets diluted. It’s not about drinking too much water-it’s about your body holding onto too much of it.
This isn’t a guess. A 2024 meta-analysis of over 30 studies found that 1.9% to 4.4% of people on SSRIs develop hyponatremia. For those over 65, the risk jumps to nearly 1 in 6. That’s not a small number. It’s a major safety issue.
Who’s Most at Risk?
Not everyone on SSRIs gets hyponatremia. But certain people are far more vulnerable:
- Age 65 and older: The risk is 3.7 times higher than in younger adults. Aging kidneys can’t regulate fluid as well.
- Women: Nearly two-thirds of cases occur in women, likely due to body composition and hormonal factors.
- Low body weight: People under 60 kg (about 132 lbs) have less total body water, so even small fluid shifts cause bigger drops in sodium.
- On diuretics: Thiazide diuretics (like hydrochlorothiazide) increase the risk by over 4 times. Many older adults take these for high blood pressure-often alongside SSRIs.
- Reduced kidney function: An eGFR under 60 means your kidneys aren’t filtering fluids properly.
- Rapid dose increases: Symptoms often appear within 2 to 4 weeks after starting or increasing the SSRI dose.
One case from a Reddit caregiver in March 2024 described her 82-year-old mother becoming severely confused just two weeks after starting citalopram. Her sodium dropped to 122 mmol/L. She was hospitalized. The doctor didn’t connect the dots until it was too late.
Why Is It Often Missed?
Confusion, dizziness, and fatigue look a lot like normal aging-or dementia. Many doctors assume an elderly patient’s mental fog is just part of getting older. A 2023 patient survey found only 28.7% of people were warned about hyponatremia before starting an SSRI. And 63.4% of primary care doctors didn’t know the typical onset window is 2-4 weeks.
That delay is deadly. On average, it takes 7.2 days from symptom onset to diagnosis. By then, the sodium level may already be dangerously low. One 78-year-old woman developed hyponatremia (118 mmol/L) and serotonin syndrome within 10 days of starting sertraline. She ended up in the ICU for five days.
The problem isn’t just the side effect-it’s the lack of awareness. Many patients and providers think of SSRIs as “safe.” But safety isn’t about being harmless. It’s about knowing the risks and watching for them.
How to Spot It Early
Hyponatremia doesn’t always start with seizures. The early signs are subtle:
- Mild nausea or vomiting
- Headaches that won’t go away
- Feeling unusually tired or weak
- Loss of appetite
- Confusion or trouble remembering things
- Mild balance problems or unexplained falls
If someone on an SSRI starts showing any of these-especially if they’re over 65 or on a diuretic-hyponatremia should be ruled out immediately. A simple blood test can check sodium levels. Urine tests can confirm SIADH (inappropriate ADH secretion), the mechanism behind this side effect.
Don’t wait for severe symptoms. By the time someone is disoriented or having seizures, it’s already an emergency.
What Should Doctors Do?
Current guidelines are clear:
- Test before starting: Check sodium levels within 7 days before beginning an SSRI.
- Test again at 2 weeks: That’s when levels typically drop. For high-risk patients, test monthly for the first 3 months.
- Don’t ignore mild symptoms: Nausea or headache in an elderly patient on an SSRI isn’t “just a bug.” It’s a red flag.
- Know the alternatives: For older adults, mirtazapine is a much safer option. It has less than half the risk of hyponatremia compared to SSRIs.
The American Geriatrics Society’s 2023 Beers Criteria explicitly lists SSRIs as potentially inappropriate for older adults due to hyponatremia risk. They recommend mirtazapine or bupropion instead.
SSRIs vs. Other Antidepressants: The Risk Comparison
Not all antidepressants carry the same risk. Here’s how they stack up:
| Antidepressant | Risk Compared to SSRIs | Notes |
|---|---|---|
| Citalopram | 2.37x higher | Highest risk among SSRIs |
| Sertraline | 2.15x higher | Commonly prescribed; high risk in elderly |
| Fluoxetine | 1.98x higher | Long half-life; risk persists after stopping |
| Paroxetine | 1.82x higher | Also has anticholinergic effects |
| SNRIs (venlafaxine, duloxetine) | 1.5-1.7x higher | Moderate risk; still higher than non-SSRIs |
| Mirtazapine | 0.47x (47% lower) | Safest option for older adults |
| Bupropion | 0.85x (15% lower) | Doesn’t affect serotonin; low risk |
| Amitriptyline (TCA) | 1.94x higher | Higher risk due to anticholinergic effects |
For every 1,000 older adults prescribed an SSRI, about 18.6 will develop hyponatremia. For those on mirtazapine, it’s only 6.5. That’s a number needed to harm (NNH) of 82-meaning you’d need to treat 82 people with SSRIs instead of mirtazapine to cause one extra case of hyponatremia.
What Happens After Diagnosis?
If hyponatremia is caught early (sodium 125-134 mmol/L):
- Stop the SSRI immediately.
- Restrict fluids to 800-1,000 mL per day.
- Sodium usually normalizes in 3-4 days.
If it’s severe (below 125 mmol/L):
- Go to the hospital.
- IV hypertonic saline (3%) is given slowly-no more than 6-8 mmol/L increase in 24 hours.
- Rushing correction can cause osmotic demyelination syndrome, a devastating brain injury.
Recovery takes time. Even after sodium normalizes, brain fog and fatigue can linger for weeks. And the depression? It doesn’t disappear. But switching to a safer antidepressant-like mirtazapine-often works just as well without the danger.
The Bigger Picture
SSRIs are still the most prescribed antidepressants in the U.S.-over 214 million prescriptions in 2023. But things are changing. Between 2018 and 2023, SSRI use in patients over 65 dropped by 22.3%. Meanwhile, mirtazapine prescriptions for that group rose by 34.7%.
The FDA now requires all SSRI labels to include hyponatremia warnings. The European Medicines Agency is reviewing safety data, with results expected by late 2025. And a new clinical algorithm published in March 2024 gives doctors a step-by-step tool to prevent and manage this side effect.
Still, an estimated 37.8% of mild cases go undetected in primary care. That means thousands of older adults are walking around with low sodium-undiagnosed, untreated, and at risk of falls, fractures, and cognitive decline.
What Patients and Families Should Do
If you or a loved one is on an SSRI:
- Ask your doctor: “Has my sodium been checked since I started this medication?”
- Watch for confusion, nausea, or dizziness-especially in the first month.
- If symptoms appear, don’t wait. Request a blood test.
- Ask: “Is there a safer alternative for someone my age?”
- Don’t assume confusion is just aging. It might be your medication.
Depression is serious. But so is hyponatremia. You don’t have to choose between treating one and risking the other. There are safer options. You just need to ask for them.
Can SSRIs cause confusion in elderly patients?
Yes. SSRIs can cause hyponatremia-low sodium in the blood-which leads to confusion, disorientation, and memory problems in older adults. These symptoms are often mistaken for dementia or normal aging, but they’re a direct side effect of the medication. Sodium levels below 135 mmol/L can impair brain function. If confusion appears within 2-4 weeks of starting an SSRI, hyponatremia should be tested for immediately.
Which SSRIs are most likely to cause low sodium?
Citalopram has the highest risk, followed by sertraline, fluoxetine, and paroxetine. Studies show citalopram increases hyponatremia risk by over 2.3 times compared to non-SSRI antidepressants. These drugs strongly bind to serotonin transporters, triggering excess antidiuretic hormone release. This causes the body to retain water and dilute sodium. Not all SSRIs are equal-some are safer than others, but all carry some risk in older adults.
Is mirtazapine safer than SSRIs for older adults?
Yes. Mirtazapine has a significantly lower risk of hyponatremia-about half that of SSRIs. It doesn’t work by boosting serotonin the same way, so it doesn’t trigger the same hormone response. For patients over 65, especially those with kidney issues or on diuretics, mirtazapine is recommended as a first-line alternative by the American Geriatrics Society. It’s just as effective for depression and often causes less nausea and sexual side effects too.
How long does it take for hyponatremia to develop after starting an SSRI?
Symptoms usually appear within 2 to 4 weeks after starting the medication or increasing the dose. This is why testing sodium levels at the 2-week mark is now standard for older adults. Waiting longer risks missing the window for early intervention. The longer hyponatremia goes untreated, the higher the chance of neurological damage or hospitalization.
Should I stop my SSRI if I feel confused?
Don’t stop abruptly without medical guidance. But do contact your doctor right away. Confusion, nausea, or dizziness could be signs of low sodium. A simple blood test can confirm hyponatremia. If it’s positive, your doctor will likely stop the SSRI and recommend fluid restriction or other treatments. Never ignore these symptoms-especially if you’re over 65, female, or on a diuretic.
Can hyponatremia from SSRIs be permanent?
No, if caught early. Sodium levels usually return to normal within 3-4 days after stopping the SSRI and restricting fluids. However, if sodium drops too low and is corrected too quickly, it can cause osmotic demyelination syndrome-a rare but serious brain injury that can cause permanent damage. That’s why slow correction under medical supervision is critical in severe cases. Long-term confusion or memory loss is usually due to prolonged untreated hyponatremia, not the medication itself.
Next Steps: What to Do Now
If you’re taking an SSRI and are over 65, ask for a sodium blood test-today. If you’re a caregiver for an older adult on an SSRI, monitor for subtle changes: a sudden lack of appetite, a new stumble, or confusion that comes and goes. These aren’t just signs of aging. They could be signs of a treatable side effect.
Depression deserves treatment. But it doesn’t have to come with hidden dangers. There are safer, just-as-effective options. You just need to ask for them.




Sachin Bhorde
December 15, 2025 AT 21:58Yo, this is huge. SSRIs causing hyponatremia isn't some edge case-it's systemic. I've seen it in my geriatric rotations: 80-year-old grandma on citalopram, starts stumbling, doc says 'oh, just aging'. Bloodwork shows Na+ at 121. She was hospitalized for 5 days. The kicker? No one checked her sodium before prescribing. We need mandatory baseline labs for anyone over 60 on SSRIs. It's not optional anymore. #MedEdFail
Joe Bartlett
December 16, 2025 AT 07:04Bit of a fuss over nothing really. We’ve been giving SSRIs for decades. People get a bit woozy, they drink too much water, end up with low sodium. Simple fix: don’t chug water. Also, Americans love overmedicating everything. In the UK, we’d just get them walking in the park and call it a day.
Chris Van Horn
December 16, 2025 AT 12:59Let me be perfectly clear: this post is not merely informative-it is a clarion call to the medical establishment’s abysmal failure in pharmacovigilance. The fact that a 2024 meta-analysis is required to reiterate what was known in 1998 speaks to the institutional rot in primary care. Furthermore, the omission of the fact that SIADH is a class effect of serotonin reuptake inhibition-rather than a drug-specific anomaly-is a glaring scholarly lapse. This is not a side effect. It is a pharmacodynamic inevitability. And yet, the FDA’s labeling remains… inadequate.
Virginia Seitz
December 17, 2025 AT 21:40OMG this is so important!! 😭 My uncle was on sertraline and started forgetting his own birthday. We thought it was dementia… turns out his sodium was 124. He’s on mirtazapine now and back to his old self! 🙌 Please, if you’re on an SSRI and feeling off-get tested!!
Peter Ronai
December 18, 2025 AT 14:52Of course SSRIs cause hyponatremia. What did you expect? These drugs are basically chemical sledgehammers to the brain’s regulatory systems. And yet, psychiatrists still treat them like aspirin. Meanwhile, the pharmaceutical industry keeps pushing them like candy. Mirtazapine? Bupropion? Too expensive. Too complicated. Too… honest. We’d rather keep prescribing the dangerous stuff because it’s profitable. Wake up.
Steven Lavoie
December 19, 2025 AT 14:33I’ve been a geriatric nurse for 22 years. I’ve seen too many cases where hyponatremia was dismissed as 'just confusion.' But here’s the thing-it’s not just about sodium. It’s about how we treat older adults. We assume their brains are 'worn out,' so we don’t look for reversible causes. This post is a wake-up call. Test sodium. Ask questions. Don’t accept 'aging' as an answer. Your loved one deserves better.
Michael Whitaker
December 21, 2025 AT 08:02It’s interesting how this post assumes that all clinicians are unaware. I’ve been prescribing mirtazapine to elderly patients since 2019-primarily because of this exact risk profile. The fact that you’re surprised suggests you’ve been operating in a bubble. Also, why are you so focused on SSRIs? TCAs have higher anticholinergic burden. SNRIs cause hypertension. Every drug has trade-offs. The key is individualized risk assessment-not blanket fearmongering.
Kent Peterson
December 23, 2025 AT 06:19Wait-so you’re saying SSRIs are dangerous? Shocking. Next you’ll tell me smoking causes cancer. And you want us to stop prescribing them? Are you insane? My cousin took fluoxetine for 12 years and is fine. Meanwhile, you’re scaring people away from life-saving treatment. This isn’t ‘awareness’-it’s fear-mongering dressed up as medicine. The real danger? People stopping meds because of alarmist blog posts. That’s what kills.
Josh Potter
December 24, 2025 AT 05:41Bro. I’m 71. Took sertraline for 3 months. Started zoning out, forgetting where I put my keys. Thought I was going senile. Went to the doc, got a blood test-Na+ 126. They switched me to mirtazapine. Boom. Back to normal in 10 days. No more brain fog. No more falls. Don’t be like me-get tested. It’s free. It’s easy. It could save your life. 🙏
Evelyn Vélez Mejía
December 25, 2025 AT 12:18There is a metaphysical tragedy here: we have weaponized neurochemistry to treat existential despair, yet we refuse to acknowledge the biological cost. The brain is not a black box. Serotonin is not a ‘mood molecule’-it is a master regulator of homeostasis. When we hijack its reuptake, we disrupt the delicate symphony of fluid balance, renal function, and neural integrity. To call this a ‘side effect’ is to sanitize violence. This is not pharmacology. This is physiological betrayal-and we are the architects.
Meghan O'Shaughnessy
December 27, 2025 AT 07:46My mom’s on citalopram. She’s 78. Last week she started forgetting how to make coffee. I asked the doctor to check her sodium. It was 128. We switched her to mirtazapine. Two weeks later, she’s making pancakes again. Thank you for writing this. I wish I’d known sooner.