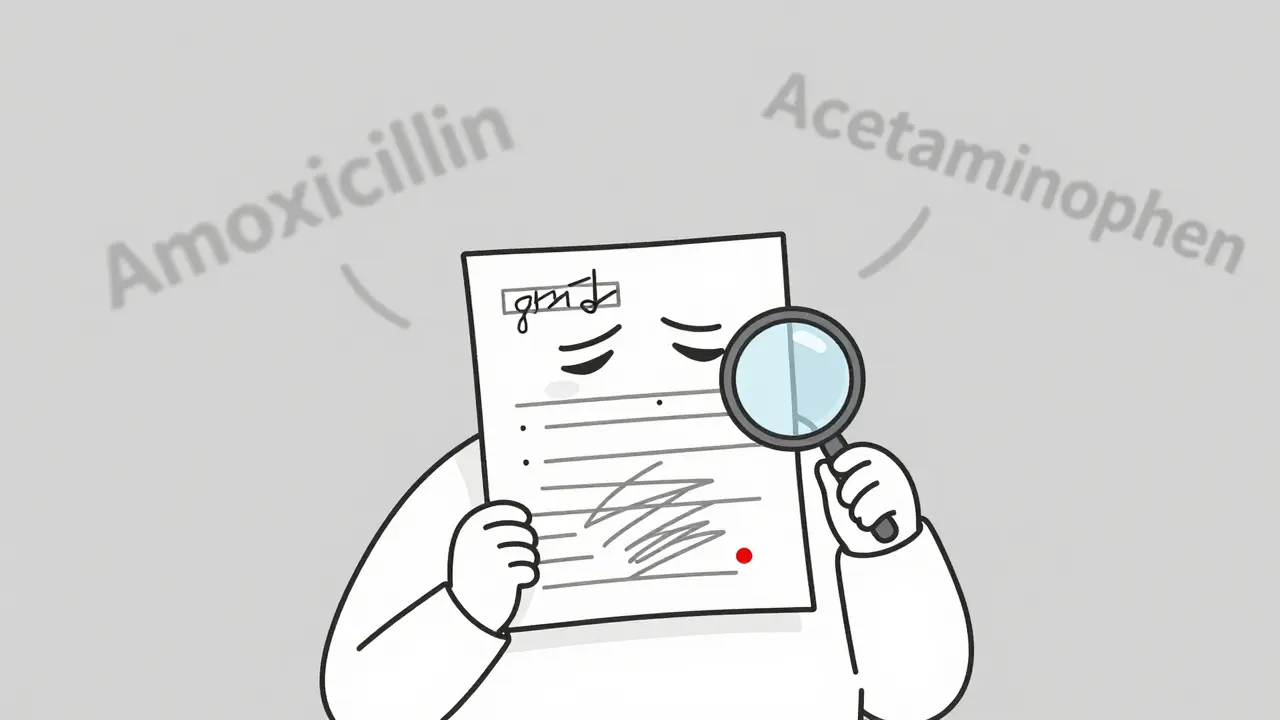
Imagine this: a pharmacist stares at a prescription, squinting at a scribble that might say amoxicillin or acetaminophen. One letter off. One misread digit. And suddenly, a patient gets the wrong drug, the wrong dose, or worse - nothing at all. This isn’t fiction. It’s happening every day in hospitals, clinics, and pharmacies around the world. Illegible handwriting on prescriptions isn’t just annoying - it’s deadly.
Why Bad Handwriting Kills
In the U.S. alone, an estimated 7,000 people die each year because doctors’ handwriting was too hard to read. That’s not a typo. That’s from the Institute of Medicine. Another 1.5 million adverse drug events happen annually due to preventable errors, and nearly a quarter of them trace back to messy handwriting. These aren’t rare mistakes. They’re systemic. Think about the numbers: 92% of medical students and doctors admit to making prescription errors. On average, each one makes two mistakes per shift. Nurses spend over 12 minutes per illegible script just trying to figure out what the doctor meant. Pharmacists make 150 million calls to doctors every year just to clarify a single line. That’s not efficiency. That’s chaos. The problem isn’t just poor penmanship. It’s the hidden dangers: missing initials, wrong dosages, confusing abbreviations like “qd” (which some read as “every day” and others as “four times a day”), or drug names that look alike - hydroxyzine vs. hydralazine. One wrong letter. One wrong number. One delayed clarification. And a patient ends up in the ER - or worse.The Human Cost of Scribbles
It’s not just about mistakes. It’s about trust. When a nurse has to guess what a doctor wrote, they’re forced to choose: call the doctor and delay treatment, or guess and risk harm. Many do both. Studies show 22% of healthcare workers admit they sometimes ignore illegible prescriptions altogether. That’s not negligence - it’s survival. When you’re running between 15 patients and your shift is already 2 hours over, you do what you can. Patients pay the price. Delays in treatment. Unnecessary tests. Wrong medications. All because a doctor wrote too fast. One study found that only 24% of handwritten operative notes in a British hospital were rated as “excellent” or “good” by nurses and pharmacists. Over a third were labeled “poor.” That’s not a bad day. That’s the norm. And it’s not just doctors. Medical trainees know the risks. A 2017 survey found 68% of students believed improving their handwriting would take too much time during patient visits. They’re not lazy. They’re overwhelmed. But the system hasn’t changed to match their reality.Enter E-Prescribing: The Real Solution
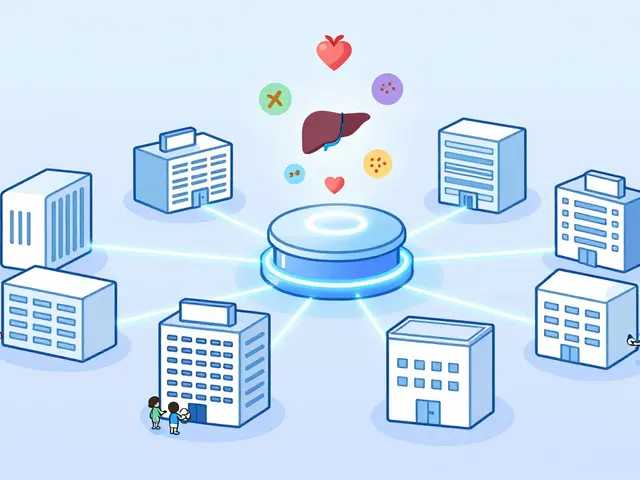
There’s a fix. And it’s not asking doctors to write neater. It’s not training nurses to guess better. It’s technology: electronic prescribing, or e-prescribing. Since 2003, e-prescribing has been slowly replacing paper. By 2019, 80% of U.S. office-based providers were using it. And the results? Stunning. A 2025 study in JMIR compared safety compliance between handwritten and electronic prescriptions. Handwritten? Only 8.5% met safety standards. E-prescriptions? 80.8%. Even when clinicians typed prescriptions manually - without templates - they still hit 56% accuracy. That’s over six times safer than scribbles on paper. E-prescribing cuts errors from illegibility by 97%. That’s not a marketing claim. That’s data from Veradigm, a major health tech firm. No more guessing what “5 mg” means. No more confusing “U” for “unit” with “0.” No more ambiguous “q4h” vs. “q6h.” The system enforces correct dosing, checks for allergies, flags dangerous drug interactions, and sends the order directly to the pharmacy. It’s not magic. But it’s the closest thing we have.
What E-Prescribing Fixes - and What It Doesn’t
E-prescribing doesn’t just fix handwriting. It fixes the whole chain. - It stops look-alike, sound-alike drug mix-ups by auto-suggesting correct names. - It blocks unsafe doses before they’re sent. - It records who ordered what, when, and why - no more “I thought they said…” - It integrates with electronic health records so everyone sees the same info. But it’s not perfect. Some doctors complain it takes longer to enter prescriptions. Others say alert fatigue is real - when the system pops up too many warnings, clinicians start ignoring them. One study found that overused alerts can make safety features less effective. That’s not a flaw in e-prescribing. It’s a flaw in how it’s designed. Good systems learn. They prioritize alerts. They adapt to your workflow. Bad ones just flood you with noise. The difference between a life-saving tool and a frustrating burden? Implementation.What If You Can’t Go Digital Yet?
Not every clinic can afford a $20,000 e-prescribing system. Not every hospital has the IT staff to train 50 doctors. In rural areas, resource-limited settings, or developing countries, paper is still the only option. So what do you do? There are still steps you can take to reduce risk:- Print, don’t cursive. Block letters are easier to read than looping handwriting.
- Avoid dangerous abbreviations. No “U” for unit. No “qd,” “qod,” or “cc.” Use “daily,” “every other day,” “mL.”
- Write everything. Patient name, drug name, dose, frequency, route, duration, and your signature. Skip one, and someone has to guess.
- Use numbers, not words. “5 mg” is clearer than “five milligrams.”
- Double-check. If you’re unsure, ask a colleague to glance at it before sending it out.





Bradford Beardall
January 10, 2026 AT 05:45Been working in a rural ER for 12 years. Saw a kid nearly die because a doctor wrote '0.5 mg' like it was '5 mg'. The pharmacist called three times. No one answered. We had to reverse it with naloxone. E-prescribing isn't optional anymore. It's basic human decency.
Christine Milne
January 10, 2026 AT 07:15Let’s be clear: this isn’t about technology. It’s about the erosion of professional standards. In my time at Johns Hopkins, handwritten prescriptions were a badge of honor. They demonstrated experience, authority, and clinical intuition. To replace that with a computer interface is to infantilize the medical profession. The real problem is lazy training, not penmanship.
McCarthy Halverson
January 12, 2026 AT 06:25Just start printing. No abbreviations. Double check. Done. No need for fancy systems if you slow down for five seconds.
chandra tan
January 13, 2026 AT 09:05India still uses paper everywhere. We use colored pens - red for antibiotics, blue for painkillers. It’s crude but it works. Also, we shout the dose out loud when handing it to the pharmacist. Sounds crazy? It’s saved lives.
Jake Nunez
January 14, 2026 AT 18:35My aunt got the wrong drug because the doctor wrote 'metoprolol' like 'metformin'. She ended up in ICU. E-prescribing should be mandatory everywhere. No excuses.
Michael Marchio
January 14, 2026 AT 18:44Let’s not pretend this is about safety. This is about corporate control. Big Pharma and EHR vendors are pushing e-prescribing because they want to lock you into their ecosystems, track every prescription, and upsell you on branded drugs. The '97% error reduction' statistic? Cooked. They only measure the obvious typos, not the hidden biases built into the algorithm. You think your computer won’t push fentanyl because it's cheaper than gabapentin? Think again.
Jake Kelly
January 15, 2026 AT 06:50I’ve seen both sides. Handwritten scripts in a busy clinic, then e-prescribing after we upgraded. The difference in stress levels? Night and day. Nurses stop looking like they’re about to cry. Pharmacists smile. Patients get their meds faster. It’s not perfect, but it’s better. And better is enough to start with.
Ashlee Montgomery
January 17, 2026 AT 03:01What if the real issue isn’t the pen or the computer but the time we take to connect with the patient before writing the script? If we’re rushing because the clock is ticking, no system will fix that. The tech helps, sure. But the humanity? That’s on us.
neeraj maor
January 17, 2026 AT 23:04They say e-prescribing reduces errors. But what if the real danger is centralized control? Who owns the data? Who decides what drugs get flagged? What if the algorithm is trained on biased datasets that favor expensive brand names? This isn’t progress. It’s surveillance disguised as safety. And they’ll come for your paper scripts next. You think this is about medicine? It’s about power.