What Are Immune-Related Adverse Events (irAEs)?
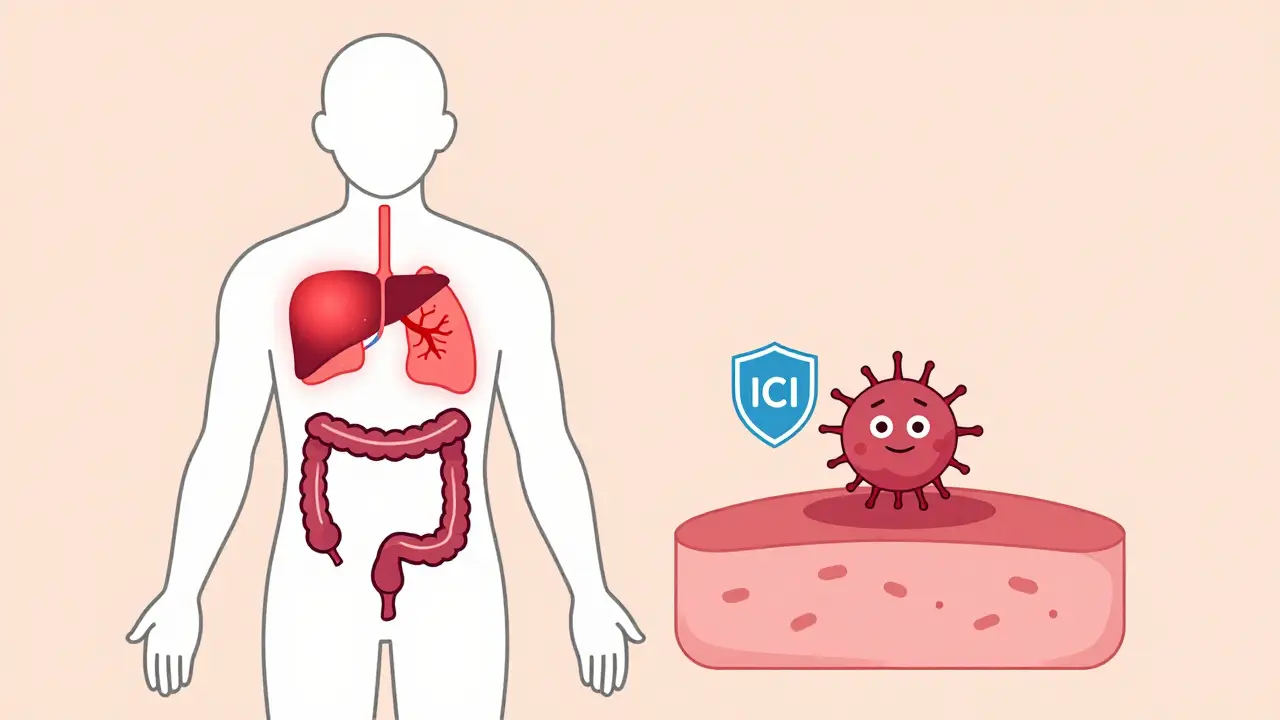
When cancer patients receive immune checkpoint inhibitors (ICIs), their immune system gets a powerful boost to attack tumors. But sometimes, that boost goes too far. Instead of just targeting cancer cells, the immune system starts attacking healthy tissues - leading to something called immune-related adverse events, or irAEs. These aren’t typical chemo side effects like nausea or hair loss. They’re autoimmune reactions - the body turns on itself.
irAEs became a recognized problem after the FDA approved ipilimumab in 2011 for melanoma. Since then, as ICIs have been used for lung, kidney, bladder, and other cancers, irAEs have become common. About 83% of patients on CTLA-4 inhibitors, 72% on PD-1 inhibitors, and 60% on PD-L1 inhibitors will experience at least one irAE. The good news? Most are manageable. The challenge? Recognizing them early - before they become serious.
How irAEs Present: It’s Not One-Size-Fits-All
irAEs can show up in almost any organ. But some are far more common than others. Gastrointestinal issues like diarrhea and colitis are the most frequent. Then come skin rashes, thyroid problems, and liver inflammation. Less common but far more dangerous? Heart inflammation (myocarditis), lung inflammation (pneumonitis), and neurological problems like nerve damage or brain swelling.
Timing matters too. Most irAEs show up within the first three months of treatment. But some don’t appear until weeks or even months after stopping therapy. A patient might feel fine after finishing a six-month course of pembrolizumab - then develop severe fatigue and joint pain two months later. That’s not a relapse. That’s an irAE.
What makes irAEs tricky is that they mimic other conditions. Diarrhea could be an infection. Fatigue could be cancer progression. A rash might look like a drug allergy. That’s why doctors don’t jump to conclusions. They rule out infections, other medications, or cancer-related causes before saying, "This is an irAE."
Grading Severity: From Mild to Life-Threatening
Not all irAEs are created equal. Doctors use the Common Terminology Criteria for Adverse Events (CTCAE) to grade them from 1 to 4:
- Grade 1: Mild symptoms. No treatment needed beyond monitoring. A little rash? A slightly elevated liver enzyme? Keep going with treatment.
- Grade 2: Moderate. Symptoms interfere with daily life. This is when treatment usually gets paused and corticosteroids start.
- Grade 3: Severe. Hospitalization may be needed. High-dose steroids are required.
- Grade 4: Life-threatening. ICU-level care. This is rare - but deadly if missed.
Grade 2 and above trigger immediate action. Delaying treatment can turn a manageable rash into a life-threatening colitis or pneumonitis. That’s why oncology teams now train nurses and patients to recognize red flags - like more than four loose stools a day, shortness of breath at rest, or new weakness in limbs.
The Gold Standard: Steroids and How to Use Them
For most irAEs, the first-line treatment is corticosteroids. But dosing isn’t one-size-fits-all.
For Grade 2-3 irAEs, doctors start with oral prednisolone at 1 mg per kg of body weight per day. That’s about 60-80 mg for a 70 kg adult. Treatment continues until symptoms drop to Grade 1, then they begin a slow taper. This isn’t a quick fix. Tapering takes 4 to 6 weeks. Rush it, and symptoms bounce back.
For Grade 3-4, it’s urgent. Patients get intravenous methylprednisolone - 1 to 2 mg per kg daily (up to 1,000 mg per day) - for 3 days. Then they switch to high-dose oral prednisolone. This isn’t just about comfort. It’s about survival. A 2023 study showed that patients who got IV steroids within 24 hours of Grade 3 symptoms had a 50% lower risk of hospitalization.
But steroids come with their own problems. Insomnia. Weight gain. Mood swings. A 2023 survey of patients found that 72% had trouble sleeping, 65% gained noticeable weight, and 58% felt anxious or depressed. Many patients say the side effects feel worse than the cancer.
What If Steroids Don’t Work?
Not all irAEs respond to steroids. About 10-15% of patients don’t improve after 48 hours. These are called steroid-refractory cases. When that happens, doctors turn to stronger immunosuppressants.
Infliximab - a drug that blocks TNF-alpha - is the go-to for colitis and some forms of pneumonitis. Mycophenolate mofetil is often used for liver or lung involvement. IVIG (intravenous immune globulin) helps with neurological irAEs. Cyclophosphamide is reserved for the toughest cases.
New data from 2024 shows vedolizumab, originally used for Crohn’s disease, works better than infliximab for steroid-refractory colitis. In a phase II trial, 68% of patients responded to vedolizumab versus 52% with infliximab. This is changing guidelines fast.
What’s critical? Don’t wait. If steroids fail, switch within 48 hours. Every day of delay increases the risk of permanent organ damage.
Special Cases: Endocrine, Neurological, and Cardiac irAEs
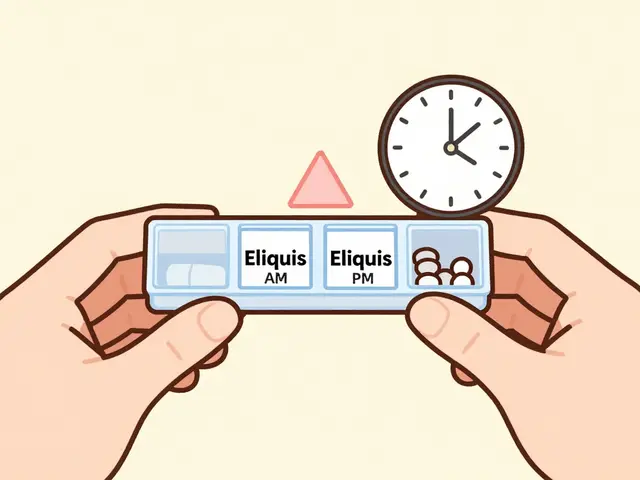
Some irAEs don’t respond to steroids the same way. Endocrine problems - like thyroid dysfunction or hypophysitis - need hormone replacement, not immunosuppression. A patient with low cortisol? They need lifelong hydrocortisone. A patient with low thyroid hormone? Lifelong levothyroxine.
Neurological irAEs - like Guillain-Barré syndrome or encephalitis - are rare but deadly. They require neurologists on the team. Dr. Jacob Brahmer from Johns Hopkins says: "Specialist neurology input is vital." Delayed treatment can lead to permanent paralysis or death.
Myocarditis? It’s the most feared. Only 3% of cardiac irAEs occur, but they cause 2.7% of all ICI-related deaths. Symptoms? Chest pain, irregular heartbeat, sudden shortness of breath. If suspected, stop ICIs immediately. Start IV steroids. Call cardiology. Get an MRI. This isn’t something to wait on.
Why Timing and Teamwork Matter
Managing irAEs isn’t just about drugs. It’s about speed and coordination.
Leading cancer centers now have dedicated immune toxicity teams - nurses, pharmacists, endocrinologists, gastroenterologists, neurologists - all on standby. At MD Anderson, 92% of patients get the right treatment on time. In community clinics without these teams? Only 68% do.
That gap saves lives. A 2022 study showed community centers that implemented structured irAE protocols cut severe complications by 37% in just 18 months. How? They trained staff. They built fast-referral pathways. They kept steroids on hand 24/7.
And they educated patients. A 2023 survey found that 79% of oncology nurses said patients didn’t understand when to call. Many thought, "It’s just a rash - I’ll wait." That’s why clinics now give patients printed guides: "Call immediately if you have: more than 4 watery stools a day, chest pain, new numbness, or trouble breathing."

The Future: Predicting, Preventing, and Personalizing Care
Researchers are now looking beyond treatment - toward prediction and prevention.
A 2023 study in Nature Medicine found that patients with baseline IL-17 levels above 5.2 pg/mL had a 4.7-fold higher risk of severe irAEs. That’s a potential biomarker. Soon, before giving ICI therapy, doctors might run a simple blood test to see who’s at high risk.
Flatiron Health’s real-world data showed that patients who got treated within 48 hours of symptom onset cut their hospitalization risk by nearly half. Early = better.
And the pipeline is growing. Over 287 ICI combinations are in trials. More combinations mean more irAEs. By 2028, specialized irAE clinics are projected to grow 22% annually. The European Society for Medical Oncology is now rolling out patient education materials in 15 languages because 41% of patients still don’t know what to watch for.
What Patients Need to Know
If you’re on an immune checkpoint inhibitor:
- Know your symptoms. Don’t ignore them.
- Call your oncology team at the first sign of trouble - even if it seems minor.
- Don’t stop steroids on your own. Tapering must be slow.
- Ask for a copy of your irAE management plan. Most clinics now give one.
- Remember: treating irAEs doesn’t hurt your cancer treatment. In fact, studies show you’re just as likely to beat cancer if you get the right irAE care.
irAEs aren’t a reason to avoid immunotherapy. They’re a reason to be prepared.
Can immune checkpoint inhibitors cause long-term damage?
Yes, but it’s rare. Most irAEs resolve completely with treatment. However, about 10-15% of patients develop chronic issues - like permanent thyroid dysfunction, adrenal insufficiency, or diabetes - that require lifelong hormone replacement. Neurological or cardiac damage can also be permanent if not treated early. That’s why early recognition and prompt treatment are critical.
Do irAEs mean the treatment isn’t working?
No. In fact, studies show the opposite. Patients who develop mild to moderate irAEs often have better cancer outcomes. The immune system is clearly active - it’s just overreacting. This doesn’t mean you should want side effects, but it does mean managing irAEs properly doesn’t reduce your chances of beating cancer.
Are irAEs more common with combination therapy?
Yes. Combining CTLA-4 and PD-1 inhibitors - like ipilimumab and nivolumab - raises the irAE rate to over 90%. The trade-off? Better cancer control. But the risk of severe irAEs also jumps. That’s why combination therapy is usually reserved for patients with aggressive cancers, and why close monitoring is non-negotiable.
Can I get irAEs after stopping immunotherapy?
Absolutely. About 15-20% of irAEs appear after treatment ends - sometimes months later. Patients often assume they’re "out of the woods" once therapy stops. That’s a dangerous assumption. If you develop new fatigue, diarrhea, rash, or joint pain after finishing ICI, tell your doctor immediately. It could still be an irAE.
What should I do if I can’t reach my oncologist?
If you have Grade 2+ symptoms - like persistent diarrhea, chest pain, trouble breathing, or neurological changes - go to the nearest emergency department. Bring your ICI treatment records. Tell them you’re on immune checkpoint inhibitors and suspect an irAE. Most ERs now have protocols for this. Don’t wait. Early intervention saves lives.
Final Thoughts
irAEs are one of the biggest challenges in modern cancer care. But they’re also one of the most manageable - if you know what to look for. With better education, faster response times, and smarter protocols, we’re turning what used to be a dangerous surprise into a predictable, treatable side effect. The goal isn’t to avoid immunotherapy. It’s to use it safely - so patients live longer, and live better.



Rob Turner
February 11, 2026 AT 23:45christian jon
February 13, 2026 AT 06:08Autumn Frankart
February 14, 2026 AT 15:29Pat Mun
February 15, 2026 AT 12:46Skilken Awe
February 16, 2026 AT 17:46andres az
February 17, 2026 AT 05:05Alyssa Williams
February 17, 2026 AT 18:15Jack Havard
February 18, 2026 AT 07:09Gloria Ricky
February 20, 2026 AT 05:05Stacie Willhite
February 21, 2026 AT 21:14Jason Pascoe
February 23, 2026 AT 08:26Annie Joyce
February 25, 2026 AT 05:54Suzette Smith
February 26, 2026 AT 00:19Sophia Nelson
February 27, 2026 AT 15:34