Blood Thinner Dose Recovery Calculator
What happened?
Enter your medication type and time missed to get guidance.
EMERGENCY WARNING
Seek immediate medical help if you experience any of these symptoms:
- Unexplained bruising or large dark patches
- Red/brown urine or black/tarry stools
- Sudden dizziness, shortness of breath, or severe headache
- Confusion or vision changes
- History of head injury with bleeding risk
Missing a dose of your blood thinner might seem like a small mistake - maybe you forgot because you were busy, or your pill organizer got mixed up, or you just didn’t feel like taking it that day. But here’s the hard truth: missing even one dose of a blood thinner can put you at real risk for a stroke, blood clot, or dangerous internal bleeding. These aren’t just medications. They’re life-saving tools that need to work exactly as prescribed. If you’ve missed a dose, you need to know what to do - and when to panic.
What Blood Thinners Actually Do
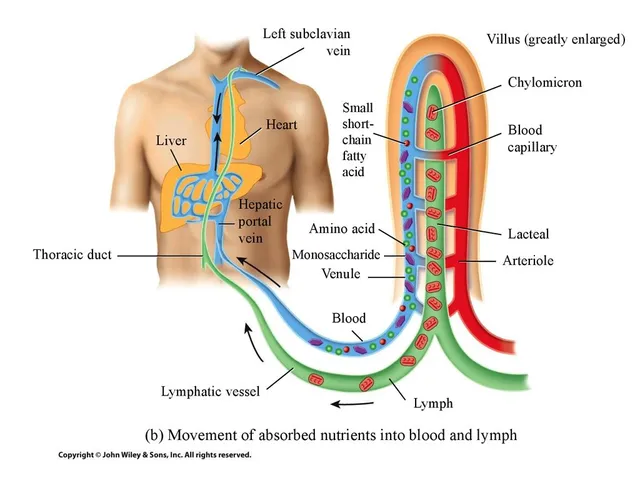
Blood thinners - also called anticoagulants and antiplatelet drugs - don’t make your blood thinner like water. Instead, they slow down your body’s ability to form clots. That’s critical if you have atrial fibrillation, a history of deep vein thrombosis, a mechanical heart valve, or have had a stroke or heart attack. Without them, clots can form in your heart or veins, break loose, and travel to your brain or lungs. That’s how strokes and pulmonary embolisms happen.
There are two main types. Warfarin (Coumadin) is the old-school option. It needs regular blood tests (INR checks) to make sure your clotting level is in the sweet spot - usually between 2.0 and 3.0. Too low? You’re at risk for clots. Too high? You could bleed internally. The newer drugs - like apixaban (Eliquis), rivaroxaban (Xarelto), and dabigatran (Pradaxa) - are called DOACs. They don’t need blood tests, but they have tighter timing rules. Apixaban, for example, must be taken twice a day, about 12 hours apart. Miss one, and your protection drops fast.
What Happens When You Skip a Dose
Let’s say you take Eliquis at 8 a.m. and 8 p.m. every day. You forget the morning dose. By noon, half the drug is already gone from your system. By 6 p.m., you’re nearly unprotected. A 2021 study in Circulation: Cardiovascular Quality and Outcomes found that when patients took DOACs less than 80% of the time, their stroke risk jumped by 57%. Warfarin is a bit more forgiving because it sticks around longer - but even then, missing doses over several days can push your INR out of range.
Real-world data from the ORBIT-AF registry shows about 1 in 8 patients miss at least one dose per month. That’s not rare. But here’s what’s scary: missed doses account for 17% to 25% of all serious complications in people on blood thinners. The risk isn’t just theoretical. It’s measured in strokes, hospital stays, and deaths.
What to Do If You Miss a Dose
There’s no one-size-fits-all answer. It depends on which drug you’re taking.
For Warfarin
- If you remember within 12 hours of your usual time: take the missed dose.
- If it’s been more than 12 hours: skip it. Don’t double up.
- Take your next dose at the regular time the next day.
- Write it down in your yellow book (your anticoagulant record).
Some guidelines say if you miss a dose before midnight, take it. After midnight, skip it. Either way, never take two doses at once. That spikes your risk of bleeding - and bleeding from warfarin can be deadly.
For Apixaban (Eliquis), Rivaroxaban, Dabigatran
- If you remember within 6 hours of your usual time: take the missed dose.
- If it’s been more than 6 hours: skip it.
- Take your next dose at the regular time.
For example: if you take Eliquis at 8 a.m. and 8 p.m., and you realize at 10 a.m. that you missed the morning dose, take it. But if it’s 2 p.m., skip it. Your body has already cleared too much of the drug. Taking it now won’t help - and could raise your bleeding risk.
One thing all sources agree on: never double up. Ever. Doubling a dose doesn’t fix the missed protection - it just increases your chance of a bleed.
When to Call Your Doctor or Go to the ER
Not every missed dose needs a panic call. But some symptoms do. If you’ve missed a dose and also notice any of these, get help right away:
- Unexplained bruising - especially large, dark patches or bruises that keep growing
- Red or brown urine - that’s blood in your kidneys or bladder
- Black, tarry stools - a sign of bleeding in your stomach or intestines
- Sudden dizziness, fainting, or shortness of breath - could mean a clot in your lungs
- A severe headache, confusion, or vision changes - possible brain bleed
- You’ve fallen or hit your head - even a minor bump can cause internal bleeding
Also, if you’ve missed more than one dose in a row, call your anticoagulation clinic or doctor. Don’t wait until your next appointment. Your protection is compromised. They may need to adjust your dose or check your blood.
And if you accidentally take too much - say, you took two pills thinking you missed one - call your doctor or go to the ER immediately. Bring your pill bottle and your yellow book if you’re on warfarin. That helps them know exactly what you took.
How to Prevent Missed Doses
The best way to avoid all this stress? Don’t miss them in the first place.
- Use a pill organizer with alarms - the ones with days of the week and morning/evening slots.
- Set phone reminders. Label them clearly: “Eliquis AM” and “Eliquis PM.”
- Refill your prescription before you run out. Don’t wait until you’re out.
- Keep your yellow book (for warfarin) with you - and update it after every dose.
- Ask a family member to check in with you once a day. A simple text: “Took your pill?” can make a difference.
- Don’t change your dose yourself. Ever. Not even if you feel fine.
People on warfarin often take it in the evening. That’s because INR tests are usually done in the morning, and evening dosing gives doctors a clearer picture. But for DOACs, timing matters more for consistency than time of day. The key is to take them at the same time every day - morning and night.
Why This Isn’t Just About Memory
It’s easy to blame yourself for forgetting. But the system is designed to fail. Pills come in different shapes. Dosing schedules vary. Warfarin needs blood tests. DOACs don’t - so people think they’re “easier.” But they’re not. They’re just different. And missing one dose of Eliquis is riskier than missing one of warfarin because it leaves your body unprotected for longer.
The American Heart Association says 1 in 5 people on blood thinners don’t take them as prescribed. That’s not laziness. It’s a system problem. We need better tools, better reminders, and better communication from doctors - not guilt trips.
But until then, you have to be your own advocate. Know your drug. Know the rules. Write them down. Stick to them. And if you’re ever unsure - call your doctor. Better safe than sorry.
What Not to Do
- Don’t stop taking your blood thinner because you’re scared of bleeding. The risk of stroke without it is far higher.
- Don’t switch brands or generics without talking to your doctor. Even small changes can throw off your balance.
- Don’t take other meds - like NSAIDs (ibuprofen, naproxen) - without checking. They can increase bleeding risk.
- Don’t assume you’re “fine” because you feel okay. Blood clots don’t always cause symptoms until it’s too late.
What should I do if I miss one dose of Eliquis?
If you miss a dose of Eliquis and remember within 6 hours of your usual time, take it right away. If it’s been more than 6 hours, skip the missed dose and take your next dose at the regular time. Never take two doses at once to make up for a missed one. Always return to your normal schedule the next day.
Can I take two doses of warfarin the next day if I miss one?
No. Never double your warfarin dose. Doing so can cause dangerous bleeding. If you miss a dose and remember within 12 hours, take it. If it’s been longer, skip it and take your next dose as scheduled. Always record missed doses in your yellow book and mention them at your next INR test.
What are the warning signs of a blood clot after missing a dose?
Watch for sudden shortness of breath, chest pain, swelling or pain in one leg (especially the calf), dizziness, fainting, or a severe headache. These could signal a pulmonary embolism or stroke. If you’ve missed a dose and have these symptoms, go to the ER immediately.
Do I need to get my blood tested if I miss a dose of a DOAC like Eliquis?
No, DOACs like Eliquis don’t require routine blood tests. But if you miss more than one dose or have symptoms of bleeding or clotting, your doctor may order tests to check your clotting status. Always report missed doses to your healthcare provider - even if you’re on a DOAC.
Can I stop taking my blood thinner if I feel fine?
Never stop taking your blood thinner without talking to your doctor. Even if you feel fine, your condition - like atrial fibrillation or a history of clotting - still puts you at risk. Stopping increases your stroke risk by up to 5 times. Your doctor will decide how long you need to take it based on your medical history.





Marie Fontaine
February 8, 2026 AT 17:54Tatiana Barbosa
February 8, 2026 AT 23:40Random Guy
February 10, 2026 AT 14:24Joseph Charles Colin
February 11, 2026 AT 02:14Brandon Osborne
February 11, 2026 AT 02:16And don't even get me started on how they treat warfarin patients like lab rats. Every other week, another needle. Meanwhile, the DOAC folks get to live like normal humans. Double standard.
Also - why is it always the patient's fault? Why isn't there an app that auto-sends a report to your doctor when you miss a dose? That's what we need. Not guilt.
Simon Critchley
February 11, 2026 AT 10:11Also - the 6-hour rule for DOACs? It’s not magic. It’s math. Apixaban’s Cmax drops 70% by 8 hours. You’re basically unprotected. Period.
And yes - I’ve seen a PE from a missed dose. It’s ugly. Don’t gamble.
Karianne Jackson
February 12, 2026 AT 20:08Andrew Jackson
February 14, 2026 AT 14:35Elan Ricarte
February 15, 2026 AT 22:54Marie Fontaine
February 16, 2026 AT 16:10Angie Datuin
February 16, 2026 AT 17:46John Sonnenberg
February 17, 2026 AT 17:28John Watts
February 19, 2026 AT 03:48Joseph Charles Colin
February 21, 2026 AT 01:11