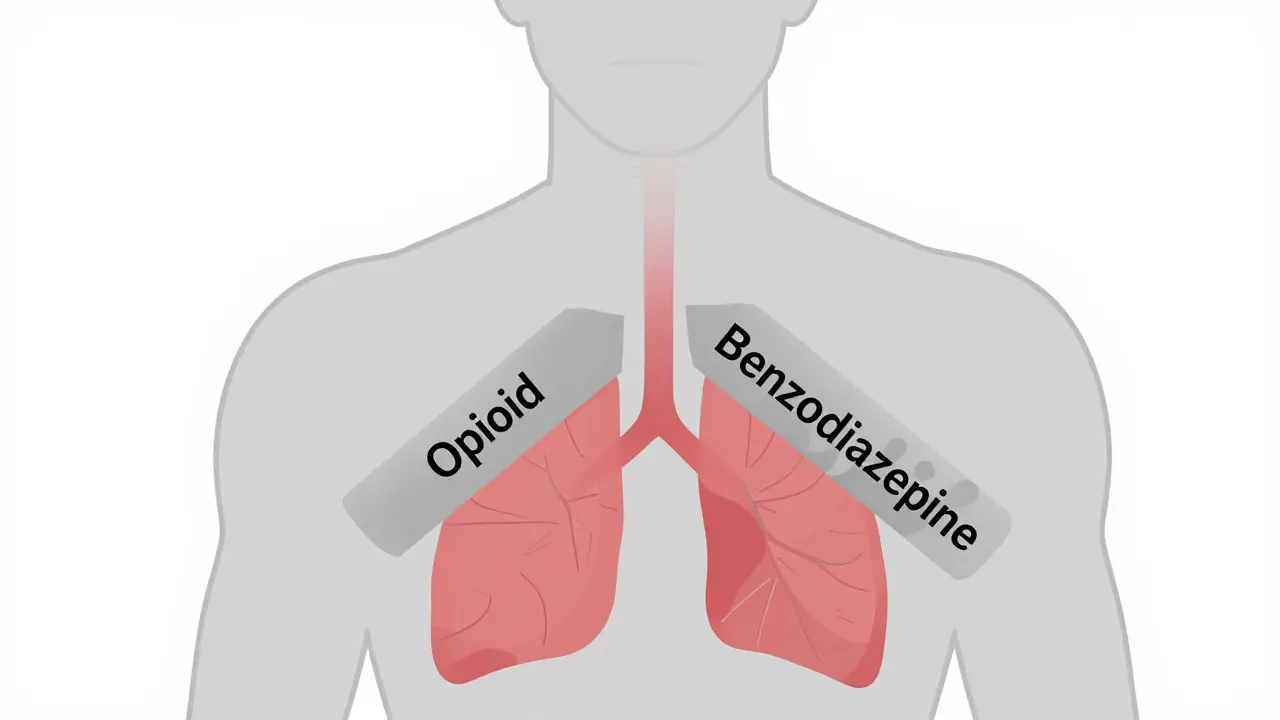
When you take opioids and benzodiazepines together, your breathing can slow down-so much that it stops. This isn’t a rare accident. It’s a predictable, well-documented danger that kills hundreds of Americans every week. The FDA first sounded the alarm in 2016, then strengthened its warning in 2019. By then, data showed that people taking both drugs were 10 times more likely to die from an overdose than those taking opioids alone. And yet, even today, this deadly mix is still prescribed far too often.
Why This Combination Is So Dangerous
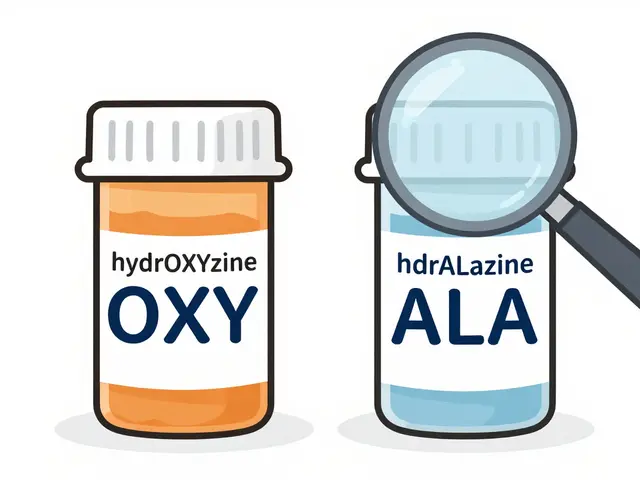
Opioids like oxycodone, hydrocodone, and fentanyl work by binding to receptors in your brainstem that control breathing. Benzodiazepines like alprazolam, lorazepam, and diazepam boost the effect of GABA, a calming neurotransmitter that also slows down brain activity, including the signals that tell you to breathe. Alone, each drug can suppress breathing. Together, they don’t just add up-they multiply. A 2021 review in the Annals of Palliative Medicine found that when people took both drugs, their blood oxygen levels dropped below 90% in 85% of cases. With opioids alone, that number was only 45%. That’s not a small difference. It’s the gap between feeling drowsy and slipping into respiratory arrest. The danger doesn’t stop at brain chemistry. Some opioids, like fentanyl and methadone, are broken down by the same liver enzyme (CYP3A4) that processes certain benzodiazepines. When you take them together, the benzodiazepine can block that enzyme, causing opioids to build up in your blood. You might be taking what your doctor calls a "normal" dose-but your body is getting a much stronger, longer-lasting hit than intended.Who’s Most at Risk
Older adults are especially vulnerable. The American Geriatrics Society lists this combination as a "potentially inappropriate" medication for people over 65. Why? Because aging slows how the body processes drugs, reduces lung capacity, and increases the chance of falls-especially when you’re sedated. A 70-year-old on oxycodone for back pain and lorazepam for anxiety isn’t just at risk for an overdose. They’re at risk for choking on their own saliva, falling, breaking a hip, and never recovering. People with sleep apnea are also in extreme danger. Both opioids and benzodiazepines relax the muscles in your throat, making airway blockages worse. One study showed that patients with sleep apnea who took both drugs had up to 15 times more breathing pauses per hour than those taking either drug alone. Even people who’ve been on opioids for years aren’t safe. Many assume they’ve built up a tolerance-that their bodies can handle more. But tolerance to the pain-relieving effects doesn’t protect you from the breathing suppression caused by benzodiazepines. A person who’s been on high-dose opioids for years can still die from a single dose of alprazolam if they’re not careful.What Happens During an Overdose
An overdose from this combination doesn’t always look like a movie scene. There’s no dramatic collapse. Often, it starts quietly: extreme drowsiness, slurred speech, confusion, slow breathing. The person might seem like they’re just "really tired." But their body is shutting down from the inside. Oxygen levels drop. Carbon dioxide builds up. The brain stops sending signals to breathe. Within minutes, the person slips into unconsciousness. If they’re alone-sleeping, watching TV, lying down-they may not be found in time. Emergency responders often arrive to find someone with shallow, irregular breaths, blue lips, and no response to pain. In 2020, 16% of all opioid-related overdose deaths in the U.S. involved benzodiazepines. That’s about 220 people every day. Many of them were prescribed both drugs by the same doctor. Some were taking them as directed. Others were using them as they were told to.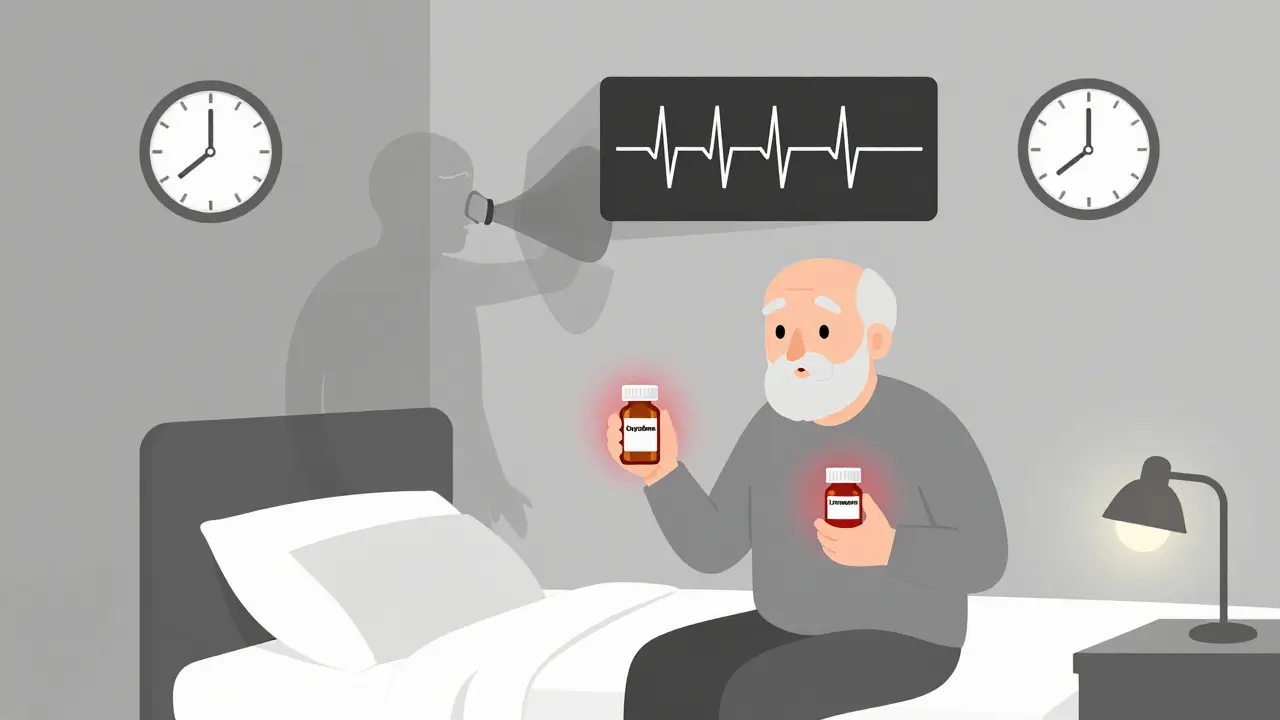
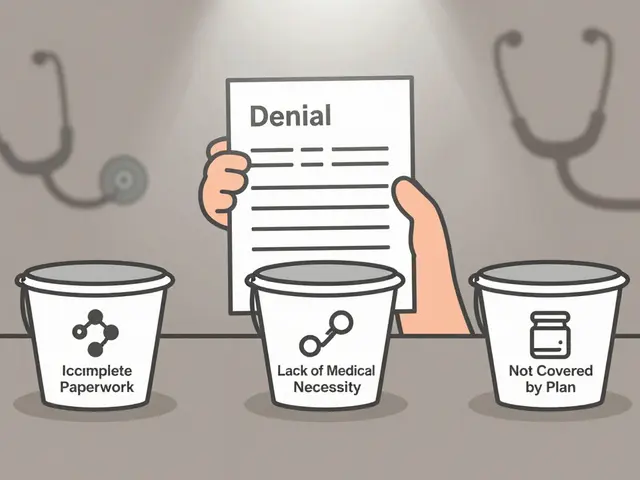
What Doctors Are Supposed to Do
The FDA says this combination should only be used when no other options exist. Even then, they recommend starting with the lowest possible dose of both drugs and monitoring closely. If a patient is already on an opioid and needs a benzodiazepine, the doctor should lower the opioid dose first. If a patient is on a benzodiazepine and needs an opioid, the opioid should be started at half the usual dose. The CDC’s 2022 guidelines say clearly: "Avoid prescribing benzodiazepines concurrently with opioids whenever possible." Many hospitals now use electronic alerts in their systems to flag when a doctor tries to write a prescription for both. One study showed these alerts cut dangerous co-prescribing by nearly 30%. But warnings don’t always reach the right people. A 2021 study of Medicare patients found that 15% of those on long-term opioids were also getting benzodiazepines. That’s millions of people. And 4.3% of them were on high-risk combinations-extended-release opioids with long-acting benzos-exactly the kind that stay in the system the longest and carry the highest danger.What You Should Do If You’re Taking Both
If you’re on opioids and benzodiazepines together, don’t panic. But do act. First, talk to your doctor. Ask: "Is this combination absolutely necessary? Are there safer alternatives?" There are non-addictive pain relievers like gabapentin or physical therapy for chronic pain. For anxiety, cognitive behavioral therapy (CBT) or SSRIs often work better than benzodiazepines in the long run. If you can’t stop one of the drugs right away, don’t quit cold turkey. Stopping benzodiazepines suddenly can cause seizures. Stopping opioids suddenly can trigger severe withdrawal-sweating, vomiting, rapid heartbeat, insomnia. Both require a slow, supervised taper. Keep naloxone on hand. Naloxone (Narcan) can reverse an opioid overdose, but it doesn’t work on benzodiazepines. Still, if opioids are part of the mix, naloxone could save your life. Make sure someone you live with knows how to use it. Never drink alcohol or take other sedatives-sleep aids, muscle relaxers, even some over-the-counter cold medicines-while on this combination. Each one adds another layer of risk.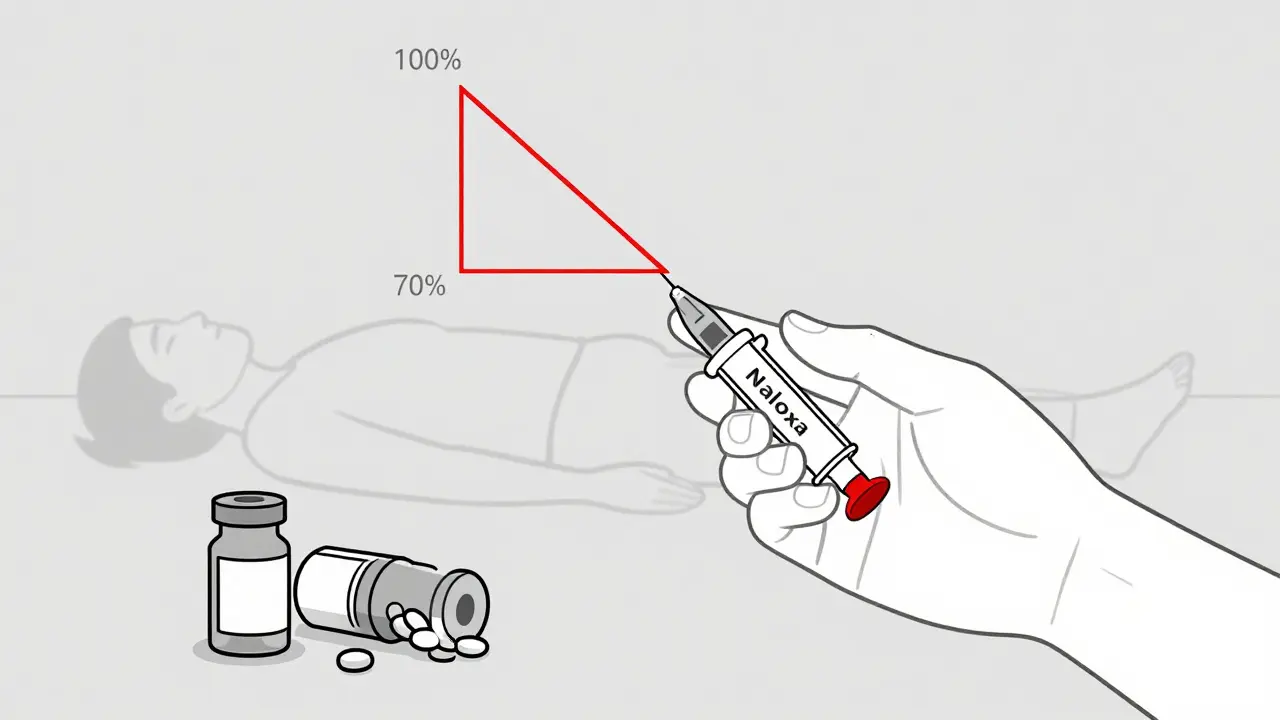
What to Watch For
Know the warning signs:- Unusual drowsiness-even after a full night’s sleep
- Difficulty staying awake during conversations
- Shallow or slow breathing (fewer than 10 breaths per minute)
- Blue lips or fingertips
- Confusion, slurred speech, or inability to wake up
The Bigger Picture
This isn’t just about bad prescriptions. It’s about a system that often treats pain and anxiety as separate problems-when they’re often connected. A person with chronic pain might develop anxiety. A person with anxiety might turn to opioids for sleep. The medical system sometimes responds by prescribing both drugs, without fully understanding the risk. Research is now focused on finding safer alternatives. New pain medications are being developed that don’t affect breathing. Better screening tools are being tested to identify who’s most vulnerable. And more doctors are learning to treat the root causes-instead of just the symptoms. But until then, the message is clear: combining opioids and benzodiazepines is one of the most dangerous things you can do to your body. It doesn’t just increase risk. It multiplies it. And the cost is measured in lives.Can I take opioids and benzodiazepines if my doctor says it’s okay?
Even if your doctor prescribes both, the risk remains high. The FDA and CDC recommend this combination only when no other options exist-and even then, with extreme caution. Always ask if safer alternatives are available. Never assume that a prescription means it’s safe. The goal is to use the lowest dose for the shortest time possible.
Does naloxone work if I overdose on both drugs?
Naloxone reverses opioid overdoses, but it has no effect on benzodiazepines. If opioids are part of the mix, naloxone can still save your life by restoring breathing. But if benzodiazepines are the main driver of sedation, you’ll still need emergency medical care. Always call 911-even if you’ve given naloxone.
How long does the risk last after I stop one of the drugs?
The risk doesn’t disappear immediately. Opioids like methadone can stay in your system for days. Long-acting benzodiazepines like diazepam can linger for over a week. Even after you stop one drug, the other can still depress your breathing. Wait at least 7-10 days after stopping either before starting the other, and only under medical supervision.
Can I use marijuana or CBD with opioids or benzodiazepines?
Marijuana and CBD can also cause sedation and slow breathing, especially in higher doses. Combining them with opioids or benzodiazepines increases the risk of overdose. There’s no safe level of mixing these substances. If you’re on either drug, avoid cannabis products unless your doctor has specifically approved it-and even then, proceed with caution.
Why do some doctors still prescribe both if it’s so dangerous?
Some doctors aren’t fully aware of the latest guidelines. Others are overwhelmed, short on time, or treating patients who’ve been on these drugs for years. Some believe the patient needs both to function. But research shows that most patients can be safely transitioned to alternatives. The rise of electronic alerts and updated training is helping, but change takes time. Don’t rely on your doctor to know everything-ask questions and do your own research.



Hayley Ash
December 31, 2025 AT 12:13So let me get this straight - the FDA warned us in 2016 and again in 2019 and yet doctors are still writing these prescriptions like they’re giving out free candy at a Halloween parade? I mean sure, maybe they’re just trying to keep their patients quiet but at what cost? A 10x increase in death risk and nobody’s getting fired? This isn’t medical negligence - it’s institutional laziness with a side of profit motive.
And don’t even get me started on the "it’s prescribed so it’s safe" crowd. If I gave my cat a Xanax and a Percocet and it died, I’d be charged with animal cruelty. But if a doctor does it to a human? They get a raise and a coffee mug that says "Patient Advocate."
kelly tracy
December 31, 2025 AT 13:50This is why America’s healthcare system is a dumpster fire. You get prescribed two deadly drugs like they’re vitamins and then told to just "ask your doctor" like that’s some kind of magic solution. Meanwhile, the doctor’s office is booked solid with 10-minute appointments and the pharmacist is too busy scanning prescriptions to even look up drug interactions.
It’s not about education. It’s about revenue. Benzodiazepines and opioids are cash cows. Insurance pays for them. Patients don’t complain because they’re too sedated to notice they’re dying slowly. And the system? It loves it. Keep the pills flowing. Keep the bills paid.
srishti Jain
January 2, 2026 AT 06:22They prescribe this combo because it’s easy. No therapy. No follow-ups. Just write script. Patient shuts up. Doctor gets paid. Everyone wins. Except the ones who stop breathing in their sleep. They don’t win.
Cheyenne Sims
January 3, 2026 AT 09:09The assertion that this combination is "predictable" and "well-documented" is accurate, but the failure of the medical establishment to enforce existing guidelines reflects a systemic collapse in clinical governance. The FDA’s warnings, while authoritative, lack teeth in the absence of mandatory audit trails, prescriber certification, and real-time pharmacy-level intervention. Without structural reform, educational appeals remain performative.
Colin L
January 4, 2026 AT 13:20I had a friend who was on oxycodone for his back and lorazepam for his anxiety - he was 52, worked in IT, never touched alcohol, never did drugs, just tried to survive the pain and the panic. His doctor told him it was "fine" because he was "stable." Two years later, he was found on the bathroom floor, blue, with his phone still in his hand, scrolling through a YouTube video about yoga for back pain. He didn’t even make it to the hospital. His wife says he never even knew how scared he was. He just felt tired. That’s the worst part. You don’t feel like you’re dying. You just feel like you need a nap.
And now I look at every prescription my mom gets and I ask: "Is this going to kill her?" I don’t trust doctors anymore. I trust Google. And I trust people who’ve lost someone. Because the system? It doesn’t care until it’s too late.
Shae Chapman
January 5, 2026 AT 13:39This is so important 💔 I’ve seen this happen to two people I love. One survived because her brother knew how to use Narcan. The other didn’t. Please, if you’re on these meds - talk to someone. Bring someone with you to your appointment. Write down your questions. Ask about CBT. Ask about physical therapy. Ask about naloxone. You deserve to be safe. You deserve to breathe without fear. You are not alone. ❤️
Nadia Spira
January 7, 2026 AT 01:55The entire paradigm of biomedical reductionism is exposed here. Pain and anxiety are not discrete pathologies - they are emergent phenomena of somatic-psycho-social dissonance. Yet the medical-industrial complex continues to weaponize pharmacological band-aids as if neurochemistry were a dial you can turn without consequences. The CYP3A4 enzyme interaction isn’t a pharmacokinetic footnote - it’s a metaphor for the collapse of holistic care into commodified symptom management. We are not treating patients. We are optimizing dosage algorithms for profit margins. The opioid-benzo synergy is merely the most visible symptom of a system that has lost its moral compass. And until we dismantle the profit-driven logic of healthcare, every "warning" is just a performative gesture masking complicity.
henry mateo
January 8, 2026 AT 13:27i just read this and my heart is breaking. my uncle was on this combo for years. he never said anything but he was always so tired. like, always. i thought he was just getting old. turns out he was slowly being suffocated by his own meds. i didn’t even know naloxone could help with opioids until now. i’m gonna get some for my grandma. she’s on a low dose but still… better safe than sorry. thanks for posting this. really.
Kunal Karakoti
January 10, 2026 AT 07:13It’s interesting how we treat drug interactions as technical failures rather than ethical ones. The science is clear, the data is abundant, yet the response remains fragmented - individual responsibility over systemic accountability. We blame the doctor, the patient, the pharmacy - but never the structure that incentivizes convenience over care. The real question isn’t whether this combination is dangerous. It’s why we continue to normalize it. What does it say about our society when death by prescribed medication is treated as an unfortunate accident rather than a preventable failure of collective will?