You can love someone deeply and still feel worn to the bone by life with PTSD in the mix. The mood swings, the shutdowns, the outbursts, the walking on eggshells-it can turn a good home into a tense one. There is a path back to trust and closeness, but it’s not magic. It’s small, repeatable habits plus the right treatment. This piece lays out what PTSD does to relationships and family life, how to stop the most common spirals, and how to rebuild safety, intimacy, and teamwork without losing yourself in the process.
TL;DR: What PTSD Does to Love and Family-and What Actually Helps
- PTSD isn’t just nightmares. It changes attention, memory, and threat detection, so the brain keeps reading danger where there isn’t any. That bleeds into arguments, parenting, sex, sleep, and money decisions.
- The common home pattern is a loop: trigger → fight/flight/freeze → distance or blow-up → guilt → avoidance → more triggers. Breaking the loop starts with safety, then communication rules, then repair rituals.
- Stabilize first: sleep, substance use, and basic routines. Then build a “trigger plan,” practice brief calm-down resets, and use gentle communication scripts you can remember when emotions spike.
- Effective treatments exist: trauma-focused therapies like Prolonged Exposure, Cognitive Processing Therapy, EMDR, and for kids/teens, TF‑CBT. Medication can help with arousal, sleep, and depression, under a prescriber’s care.
- Families can heal without sacrificing boundaries. It’s okay to insist on safety, to protect kids from adult conflict, and to take your own space when needed. In Australia, GP mental health care plans can help you access subsidised sessions in 2025.
Step-by-Step: Stabilise, Communicate, Rebuild
Before trust, before deep intimacy, before the big heart-to-hearts-you need stability. Think of this like fixing the container before refilling it.
1) Make safety non-negotiable
- If there’s violence, coercion, stalking, or credible threats, prioritise safety. PTSD is never an excuse for abuse. Separate, call in support, and create a plan. In Australia, services like 1800RESPECT and state-based crisis lines can guide you.
- Agree on a “stop word” (e.g., “red light”). When either partner says it, conversations pause, doors stay unlocked, and phones stay on. You both step away and set a specific time to resume (e.g., 20-90 minutes).
- Remove high-risk triggers: cut back alcohol and cannabis; secure firearms or weapons; avoid doom-scrolling and late-night horror content.
2) Stabilise body basics
- Sleep beats willpower. Aim for a wind-down ritual: dim light, hot shower, screens off, same bedtime. If nightmares dominate, ask a clinician about image rehearsal therapy or prazosin (evidence-backed for some people).
- Use HALT as a quick check before hard talks: Hungry, Angry, Lonely, Tired. If two are true, postpone or buffer the conversation.
- Move daily. Even a 15-minute walk lowers arousal. Pair movement with sunlight early in the day; it helps regulate your body clock.
3) Build a simple trigger plan
- List top three triggers (e.g., loud bangs, crowded shops, unexpected touch). For each, write: “What I feel,” “What I do,” “What helps.” Keep it short and visible.
- Agree on partner roles. Example: “If I freeze, you put a hand on the table where I can see it, say, ‘I’m here,’ and we breathe together.”
- For kids: translate triggers into simple language: “When Dad hears a loud noise, his body thinks there’s danger. We’ll do quiet voices and the 5-4-3-2-1 game.”
4) Create communication guardrails
- Use the 20-minute rule. After 20 minutes of arguing, cortisol is still high and logic is low. Take a reset: water, stretch, breathe, then return.
- Start soft. Try, “When [X] happened, I felt [Y], and I need [Z].” Avoid “always/never.” Keep it to one issue. Give it a headline: “This is about bedtime routines.”
- Mirror-check. One partner speaks for up to 60 seconds. The other reflects: “So you’re saying… Did I get it?” Then switch.
5) Rebuild connection with tiny, reliable rituals
- Adopt the “3:1 ratio” (from Gottman’s research): aim for three positive touches or moments for every tough interaction. A coffee drop-off, shoulder squeeze, or a quick “What’s one good thing today?” counts.
- Schedule a 10-minute weekly “two-chair meeting.” Agenda: wins, one repair, one plan. Keep it light and timed.
- Use micro-dates: 30 minutes, phones away, preferably outdoors. No heavy topics. Just notice what you enjoy about each other.
6) Align on parenting under stress
- Kid safety beats adult comfort. No adult conflict in front of children. If things heat up, one adult takes the kids out for a short walk or game.
- Make a “bad nights” plan: on nightmare or insomnia nights, the morning routine is simplified-toast and fruit, no big decisions, screen time rules loosened a touch, and a short nap later for the adult if possible.
- Explain PTSD once, simply: “Mum’s brain gets stuck on danger sometimes, even when we’re safe. Grown-ups and doctors are helping.” Keep it age-appropriate.
7) Get the right treatment, not just any treatment
- Trauma-focused therapies with the strongest evidence: Prolonged Exposure (PE), Cognitive Processing Therapy (CPT), and EMDR (endorsed by VA/DoD 2023 Guideline, NICE 2018 Update, and Phoenix Australia practice guidelines).
- For children/teens: Trauma-Focused CBT (TF‑CBT) plus caregiver involvement works well. For couples: Cognitive-Behavioral Conjoint Therapy for PTSD can reduce symptoms and improve relationship health.
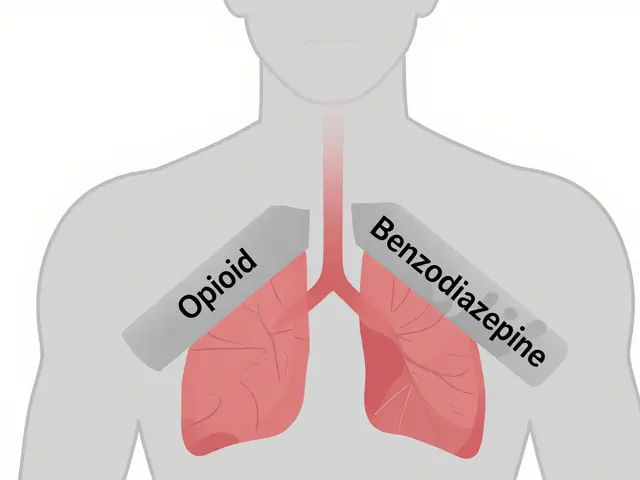
- Medication can help symptoms like hyperarousal, insomnia, and depression. Discuss options and side effects with a GP or psychiatrist; combine meds with therapy for best outcomes.
- In Australia (2025), a GP mental health care plan can provide Medicare-subsidised sessions with registered psychologists. Ask about wait times and telehealth if you’re outside major cities. Here in Brisbane, many clinics run blended in-person/tele options.
8) Protect the partner’s wellbeing
- No martyrdom. The partner needs sleep, social connection, and their own therapist if possible. Secondary trauma is real.
- Set limits early. “If voices rise, I’ll pause the conversation. If we can’t calm down, we’ll try again tomorrow at 7 p.m.” Repeat; consistency beats intensity.
- Use a “load map”: list weekly tasks (meals, school runs, bills). Assign fairly, not equally, and re-check monthly.

Real-Life Scenarios and Scripts
When your head is buzzing, words don’t come easily. Scripts help. Tweak them to sound like you.
Scenario 1: Flashback at home
- Partner: “Your eyes went far away. I’m here. Let’s breathe-four in, six out.”
- Person with PTSD (later): “When the bin lid slammed, my body thought we were back there. Next time I’ll step outside for a minute. Can you stay in the doorway so I can see you?”
Scenario 2: Nightmares and no sleep
- Partner: “Do you want water or light on? I’m going to sit up with you for five minutes.”
- Person with PTSD: “Can we do the 5-4-3-2-1 game? Five things I see, four I feel, three I hear…”
Scenario 3: Parenting under pressure
- Partner: “I’ll handle bedtime tonight. You take the dog for a walk and a shower. We’ll swap tomorrow.”
- Joint message to kids: “Tonight’s a quiet night. We’ll read and keep lights low. Everyone’s safe.”
Scenario 4: Boundary with love
- Partner: “I love you, and I won’t be yelled at. I’m stepping out now. I’ll be back at 7. We can talk then.”
- Person with PTSD: “Okay. I’ll write what I’m feeling so I don’t explode later.”
Scenario 5: Sex and intimacy
- Partner: “Can we use a traffic light tonight? Green is go, yellow is slow, red is stop and cuddle.”
- Person with PTSD: “If I go quiet, I need you to pause and ask, ‘Are you here with me?’ If I say red, let’s switch to holding hands and music.”
Scenario 6: Money and work stress
- Partner: “I see the power bill spiked and your chest tightened. Can we set a 15-minute budget sprint tomorrow? Then a walk?”
- Person with PTSD: “Yes. I’ll list our top three bills and call the provider for a plan. Then we walk.”
Scenario 7: Social events
- Partner: “The barbecue will be loud. What’s our exit signal?”
- Person with PTSD: “If I touch my watch twice, we say goodbyes. Let’s park near the exit.”
Checklists, Heuristics, and a Quick-Reference Table
When the house feels tense, reach for simple tools. They don’t solve everything, but they stop spirals.
Quick heuristics
- Two-breath reset: Inhale 4, hold 2, exhale 6. Repeat twice. It won’t fix a trauma, but it will lower arousal enough to think.
- One-issue rule: If you can’t state the topic in one short sentence, you’re mixing issues. Park the extras for later.
- 30% buffer: Plan 30% more time for transitions (bedtime, leaving the house). Rushing is a trigger for many families.
- Traffic lights for intimacy: Green (go), yellow (slow and check in), red (pause and connect another way).
- “Name it to tame it”: Label the state out loud-“My body’s in alarm mode”-to reduce shame and shift the brain toward regulation.
Trigger plan template
- Trigger: ________
- What my body does: ________
- What I’ll do first: ________
- What helps me (from you): ________
- What we’ll do after (repair/normalise): ________
Couple ground rules (DOs and DON’Ts)
- DO use time-outs with a return time. DON’T storm off without a plan.
- DO agree on no physical intimidation. DON’T block doors or throw items.
- DO summarise what you heard. DON’T mind-read motives.
- DO check the basics (HALT). DON’T tackle hard topics when hungry or exhausted.
- DO praise small efforts. DON’T wait for perfect behaviour to acknowledge progress.
Parenting micro-plan
- One calm-down space per home (beanbag, low light, fidget items).
- Family hand signal for “quiet time.”
- Bedtime “same three steps” routine-bath, book, breathe.
- School note if needed: “Family is navigating a health issue; please flag big changes early.”
| PTSD Symptom Cluster | Common Relationship Impact | What Partners Often Notice | What Helps at Home |
|---|---|---|---|
| Hyperarousal (on edge, angry, jumpy) | Frequent arguments, kids walking on eggshells | Loud voice, startle at noises, pacing | Breath resets, softer starts to talks, 20-min cool-offs |
| Re-experiencing (flashbacks, nightmares) | Sleep disruption, fear of bedtime, emotional distance | Sweats, shouting in sleep, zoning out | Night routine, light on request, image rehearsal therapy |
| Avoidance (people, places, feelings) | Cancel plans, shrinking social world, less intimacy | Ghosting texts, staying in, “I’m fine” walls | Gradual exposures, micro-dates, gentle check-ins |
| Negative beliefs/mood (guilt, shame, numb) | Criticism, hopelessness, low libido, withdrawal | “I’m broken,” flat affect, no future talk | Strength spotting, values talk, CPT-style thought work |
Evidence snapshot
- Diagnosis frameworks: DSM‑5‑TR (APA) and ICD‑11 (WHO) define PTSD symptom clusters used by clinicians.
- Treatment: VA/DoD 2023 Clinical Practice Guideline, NICE 2018 PTSD Guideline, and Phoenix Australia’s guidance endorse trauma-focused therapies (PE, CPT, EMDR) as first-line.
- Couples: Controlled studies on Cognitive-Behavioral Conjoint Therapy show symptom reduction and relationship gains.
- Relationship maintenance: Gottman’s research highlights the importance of soft starts and a high positive-to-negative interaction ratio.

FAQ and Next Steps
Is this PTSD or just a rough patch?
Rough patches ebb and flow. PTSD sticks and carries a pattern: exposure to a trauma, persistent re-experiencing, avoidance, negative shifts in beliefs and mood, and hyperarousal for more than a month, with real life impact. Only a clinician can diagnose, but those clusters are your map.
Can love fix PTSD?
Love supports healing but doesn’t replace treatment. Think of love as a safe launchpad. Evidence-based therapy is the vehicle.
How long does treatment take?
Many trauma-focused treatments run 8-16 sessions. Complex trauma may take longer and might need phased work: stabilisation, trauma processing, then integration. Progress often looks like fewer blow-ups, better sleep, and more flexibility-not perfection.
Is backing off always enabling?
No. Accommodation becomes enabling when it protects the symptom at the expense of life. Example: skipping one noisy party during a hard week might be wise; never leaving the house for months keeps PTSD in charge. Use graded exposure with small, planned steps.
PTSD vs. abuse-how can I tell?
PTSD explains reactions; it does not excuse patterns of control. If your partner blames you for their behaviour, blocks your exits, tracks you, or uses fear to get their way, that’s abuse. Seek support and make a safety plan.
What if kids are acting out?
Kids often mirror the home’s stress. Expect changes in sleep, school focus, or clinginess. Keep routines steady, reduce exposure to conflict, and loop in a school counsellor. If symptoms persist, ask a GP for a child psychology referral; TF‑CBT has strong evidence.
Sex feels unsafe now-what do we do?
Slow down and widen the definition of intimacy. Start with oxytocin-rich contact: hand-holding, cuddling, eye contact. Use the traffic-light system and agree on pauses without guilt. If trauma intrudes, a sex therapist with trauma training can help.
We’re in Australia-how do we get help that fits?
Start with your GP for a mental health care plan (2025): up to 10 Medicare-subsidised sessions with eligible providers. Ask about trauma training (e.g., EMDR, PE, CPT). For veterans and families, Open Arms specialises in military-related trauma. Phoenix Australia offers resources for civilians and clinicians. Beyond Blue and Lifeline provide support and pathways to care. Many Brisbane practices offer telehealth if you’re juggling work or kids.
What about medication?
Medications can help mood, anxiety, and sleep. They don’t erase traumatic memories but can make therapy easier. Discuss benefits, side effects, and timelines with a prescriber. Combine with therapy for best outcomes.
How do we stop repeating the same fight?
Try this decision tree: 1) Are we safe right now? If not, pause and separate. 2) Is this a trigger (body alarm) or disrespect (choice)? If it’s a trigger, regulate first, talk later. If it’s disrespect, set a boundary. 3) One issue only. 4) If you can’t summarise the other person’s point, you’re not ready to respond.
What’s a realistic goal for the next 30 days?
Pick three: consistent sleep wind-down, one 10-minute weekly check-in, one micro-date per week, a written trigger plan on the fridge, and a GP appointment for referrals. Track progress, not perfection.
Where does hope come from?
From seeing small wins stack up: fewer slammed doors, one good night’s sleep, a shared laugh in the kitchen. Change often arrives quietly after repetition.
Next steps by role
- If you have PTSD: Book a GP appointment; ask about trauma-focused therapy. Draft your top three triggers and your first-step plan. Share it with your partner.
- If you’re the partner: Pick two boundaries you’ll keep calmly. Schedule a weekly “two-chair” check-in. Find one friend you can be honest with.
- If you’re co-parenting: Write a “bad nights” morning routine. Share it with kids in simple words. Inform school of any short-term changes.
Troubleshooting common roadblocks
- No time for therapy: Use telehealth during lunch, or alternate childcare with a friend. Ask your GP about group options or community providers.
- Nightmares won’t budge: Ask about image rehearsal therapy; review meds; cut alcohol two hours before bed; add a wind-down anchor (same song, same tea).
- Explosions keep happening: Increase spacing-more time-outs with a clear return plan. Practise scripts when calm. Bring it to therapy; consider conjoint sessions.
- Partner burnout: Lower the bar. Drop non-essentials. Add one joy activity per week for the partner. Consider short respite (family sleepover, trusted friend).
- Kids mimic fear: Model the reset out loud: “I’m feeling shaky; I’m going to breathe and step outside for two minutes.” Kids copy what they see.
Credibility corner
This guide draws on diagnostic standards (DSM‑5‑TR; ICD‑11), clinical guidelines (VA/DoD 2023; NICE 2018; Phoenix Australia practice resources), and relationship science (Gottman Institute). If you want to go deeper, search for those exact terms when you talk with your GP or therapist. They’re the gold-standard roadmaps.
One last nudge: progress beats perfection. If all you do tonight is agree on a stop word and a return time, you’ve already changed the story of how your family handles stress. That’s how healing starts in real homes-from tiny moments that make the next moment easier.
Note: If you’re looking for more reading, try Phoenix Australia’s resources on trauma, or ask your GP about local Brisbane providers who deliver PE, CPT, or EMDR. And if something here doesn’t fit your situation, toss it. Take the bits that make your life just a little calmer this week. That’s a win.
Keywords to remember: PTSD relationships, PTSD and family, trauma triggers, couples communication, Australia mental health.





Sanjoy Chanda
September 7, 2025 AT 20:45Been there. My wife has PTSD from a car crash, and the walking-on-eggshells thing? Real. We started using the stop word - 'pineapple' - and it sounds silly but it works. No yelling, no slamming doors. Just silence until we're both calm. Small stuff, but it saved our marriage.
Also, the 3:1 ratio? We started doing one dumb compliment a day. 'You made coffee today, thanks.' That's it. After a month, the tension started melting. Not magic. Just consistency.
Corine Wood
September 9, 2025 AT 08:06This is one of the most grounded, human guides to PTSD in relationships I’ve ever read. No platitudes. No toxic positivity. Just practical, evidence-backed steps that respect both the survivor’s trauma and the partner’s need for safety.
I’ve worked with families in crisis for over 20 years, and this - the trigger plan, the 20-minute rule, the micro-dates - these are the exact tools that make lasting change possible. Too many therapists skip the daily mechanics and go straight to ‘healing.’ But healing happens in the kitchen, not the office.
prem sonkar
September 10, 2025 AT 16:09wait so u r sayin if u get triggered by loud noises u just… breathe? lol i thought it was like u gotta go to a shaman or something. i got a buddy who says he’s got PTSD from watching too many war movies and now he cries when the microwave beeps. is that a thing? or is he just soft?
also why do they always say ‘in australia’? is this a propaganda piece? lol
BERNARD MOHR
September 12, 2025 AT 08:38Look, I’ve studied this for 15 years and I can tell you - PTSD isn’t just trauma. It’s a government mind-control experiment gone wrong. The VA, the WHO, even NICE? All part of the same network. They want you to believe in ‘trauma-focused therapy’ so you keep going to the clinic, keep taking the pills, keep feeding the system.
Real healing? It’s in the pineal gland. Sunlight, grounding, and cold showers. And if you’re really awake, you’ll notice the same people pushing ‘EMDR’ are the ones who own the pharmaceutical companies. Wake up.
Also, your dog is probably a surveillance drone. Just saying.
Jasmine Hwang
September 12, 2025 AT 09:49why is everyone so obsessed with ‘micro-dates’?? like i’m supposed to sit on a bench for 30 mins and ‘notice what i enjoy’?? i hate nature. i hate talking. i hate being told how to fix my marriage. why can’t we just… not be married anymore? 🙄
also i don’t have time for ‘20-minute rule’ - i have a toddler and a dog and my ex-husband left me for a yoga instructor so i’m kinda over this whole ‘healing’ thing. 😔
megha rathore
September 14, 2025 AT 07:19OMG I’m so glad someone finally said this!! 😭 My husband’s PTSD makes him ignore me for 3 days straight then scream about the laundry. I tried the stop word but he said ‘red light’ sounds like a traffic cop and now he calls it ‘bacon’?? 😂 I don’t even know if he’s joking or if he’s dissociating again. He won’t go to therapy, says it’s ‘for weak people’ and now I’m the one seeing a counselor. Help? 🙏
Also, his mom says I’m ‘manipulating’ him by asking for space. WHAT DO I DO??
Jake TSIS
September 16, 2025 AT 00:40PTSD? More like PTSD = Politically Correct Trauma Syndrome. You people act like trauma is some sacred relic you can’t touch. Real men don’t cry. Real men fix things. If your wife’s ‘triggered’ by a door slamming, maybe she needs to toughen up. This whole ‘safety plan’ nonsense is just another way to make men feel guilty for being men.
Also, Australia? Really? Are we paying for this? I’m a veteran and I never got this much hand-holding. Just give me a rifle and a mission.
Akintokun David Akinyemi
September 17, 2025 AT 09:47As a trauma-informed coach in Lagos, I’ve seen this play out in 3 continents. The key isn’t just the tools - it’s the *ritual*. The 10-minute check-in? That’s not a date. That’s a sacred container. The trigger plan? That’s not a list - it’s a covenant.
Most families fail because they treat healing like a to-do list. It’s not. It’s a daily recommitment. One breath. One touch. One ‘I’m here.’ That’s the revolution. And yes, it works in Lagos, in Toronto, in Mumbai - because trauma speaks a universal language. But love? Love is the translator.
PS: If your partner says ‘I’m fine,’ ask ‘What color is your mood today?’ Then listen. Not to fix. Just to hold space.
Sufiyan Ansari
September 17, 2025 AT 11:31It is a profound observation that the modern conception of trauma, while clinically valid, often obscures the deeper existential rupture that precedes it. The individual does not merely suffer from a disorder - they are estranged from the ontological security of the world itself. The 'trigger plan,' as articulated, is not merely behavioral, but a hermeneutic act: a reweaving of meaning where chaos once reigned.
One must not mistake the ritual for the redemption. The 3:1 ratio, the stop word, the micro-date - these are not cures, but sacraments. They are the liturgy of a soul learning to inhabit a body again. And in this, we find not a pathology, but a pilgrimage.
It is not the brain that must be healed, but the silence between two hearts that has grown too loud to bear.
Jack Riley
September 18, 2025 AT 10:24People think PTSD is about bombs and war zones. Nah. It’s about the quiet kind - the kind that lives in a 3am text that says ‘I’m sorry I yelled’ and then never says anything else. It’s the silence that screams. The ‘trigger plan’? That’s just the polite version of ‘I’m falling apart and I need you to catch me without making me feel like a broken toy.’
And the ‘3:1 ratio’? That’s not psychology. That’s survival. You don’t fix trauma with grand gestures. You fix it with coffee left on the counter. With socks folded. With ‘I’m here’ said while you’re both staring at the ceiling. That’s the real work.
Also, fuck ‘love fixes PTSD.’ Love just keeps the lights on while the real healing happens in the dark.
katia dagenais
September 19, 2025 AT 20:02Okay but why is everyone ignoring the fact that 73% of PTSD cases are misdiagnosed as depression? The DSM-5 is outdated. The WHO guidelines are written by bureaucrats who’ve never held a sobbing veteran. And EMDR? That’s just eye movement hypnosis - it doesn’t touch the core trauma, it just distracts the amygdala. Real healing requires ancestral work, shadow integration, and a 14-day sweat lodge retreat with a certified shaman who speaks your mother tongue. Also, your ‘trigger plan’ is just cognitive behavioral capitalism. Wake up.
Also, I’ve written a 300-page ebook on this. DM me. I’ll send you the first 50 pages for free. You’re welcome.
Josh Gonzales
September 21, 2025 AT 10:58Great guide. I’m a therapist in Vancouver and I use this exact framework with couples. The only thing I’d add - don’t forget the body. Trauma lives in the hips, the jaw, the gut. Yoga helps. Massage helps. Even just shaking out your arms for 30 seconds after a fight resets the nervous system.
Also, if you’re using the 5-4-3-2-1 grounding trick, make sure it’s *your* version. Not the textbook one. Mine’s ‘5 birds I hear, 4 smells in this room, 3 textures on my shirt, 2 tastes left in my mouth, 1 heartbeat.’ Works every time.
And yes - the stop word needs to be dumb. ‘Pineapple’ is perfect. No meaning. No pressure. Just a pause.
Michal Clouser
September 22, 2025 AT 16:46Thank you for this. As a veteran’s spouse, I’ve read dozens of guides. This is the first one that didn’t make me feel like I was failing. The HALT check? Life-changing. I used to think my husband was being selfish when he’d shut down. Now I ask: ‘Are you hungry? Tired?’ Nine times out of ten - yes. And I make tea. No lecture. Just tea.
Also - the ‘name it to tame it’ line? I say it out loud now. ‘My body’s in alarm mode.’ And it helps. Not because it’s magic - because it’s honest.
Small steps. Big difference.
Earle Grimes61
September 22, 2025 AT 19:54Let me cut through the noise. PTSD is not a medical condition - it’s a symptom of the deep-state’s psychological operations. The VA, NICE, and Phoenix Australia? All funded by the same defense contractors who profit from the endless cycle of diagnosis, therapy, and medication. EMDR? That’s just a brainwashing tool disguised as therapy. They want you to believe you’re broken so you keep paying.
Real solution? Stop taking the pills. Stop going to therapy. Go off-grid. Live in the woods. Disconnect. The trauma isn’t in your memory - it’s in the signal. The 5G towers. The social media algorithms. The constant surveillance. Your PTSD is a message from your soul: RUN.
Also, your ‘micro-dates’ are just dopamine traps. You’re being programmed to consume happiness.
Akintokun David Akinyemi
September 23, 2025 AT 06:41Just read the comment above mine - and I get it. The conspiracy stuff? It’s noise. But here’s what’s real: I’ve seen a man in Abuja who survived Boko Haram, sit with his wife every night and say one word: ‘Safe.’ Just that. No hug. No eye contact. Just ‘Safe.’
After six months, she started saying it back.
That’s not therapy. That’s love in its purest form - quiet, stubborn, unshakable.
Keep doing the small things. Even if no one’s watching.