When doctors prescribe stimulant medications for ADHD, most families focus on one thing: Does it work? The answer is usually yes - about 70 to 80% of kids and adults see clear improvements in focus, impulsivity, and daily functioning. But behind that success story are two quieter, often overlooked risks: what’s happening to the heart, and what’s happening to sleep.
How Stimulants Affect the Heart
Stimulants like methylphenidate (Ritalin, Concerta) and amphetamines (Adderall, Vyvanse) work by boosting dopamine and norepinephrine in the brain. That’s what helps with attention. But those same chemicals also hit the nervous system that controls your heart and blood vessels. The result? A measurable, though usually small, rise in blood pressure and heart rate.
A 2025 study from the University of Southampton, the largest of its kind, looked at data from dozens of clinical trials. It found that after weeks or months of treatment, stimulants raised systolic blood pressure by 1 to 4 mmHg on average and increased heart rate by 1 to 2 beats per minute. Sounds minor? It is - for most people. But even small, steady increases can add up over time.
Long-term data from a 14-year JAMA Psychiatry study showed that people who took stimulants for ADHD had a 17% higher risk of developing cardiovascular disease, especially high blood pressure and artery problems. The risk climbed the longer they were on medication, especially during the first three years. Another study from the American College of Cardiology found that young adults on stimulants were 17% more likely to develop cardiomyopathy after one year - and 57% more likely after eight years. That doesn’t mean it’s common. The absolute risk is still very low. But it’s real.
Here’s what’s happening inside the body: stimulants can cause blood vessels to tighten (vasospasm), increase inflammation in artery walls, and, in rare cases, stretch out the heart’s electrical system, leading to irregular rhythms. A 10-beat-per-minute rise in heart rate is linked to a 20% higher chance of cardiac death. The numbers from ADHD meds don’t usually go that high - but they’re in the same direction.
Stimulants vs. Non-Stimulants: Is One Safer?
Many assume non-stimulants like atomoxetine (Strattera) or viloxazine (Qelbree) are gentler on the heart. But the 2025 Southampton study found they cause nearly the same increases in blood pressure and heart rate. The only exception? Guanfacine and clonidine. These alpha-2 agonists actually lower both blood pressure and heart rate. That’s why they’re sometimes used for kids with ADHD who also have anxiety or trouble sleeping.
That’s a key point: not all ADHD meds affect the heart the same way. Methylphenidate might carry a slightly higher short-term risk of heart attack in the first few weeks after starting - though the increase wasn’t statistically significant overall. Amphetamines? They’re linked more closely to long-term changes. And if someone already has a heart condition, family history of sudden death, or a genetic condition like Long QT Syndrome, the risks shift.
For those with Long QT Syndrome, opinions are mixed. One study of 48 patients found more fainting and heart rhythm issues. Another study of 28 kids found no serious events - and even fewer than expected. That’s why experts now say: don’t automatically say no. Do a full cardiac history. Talk to a cardiologist. Check an ECG if there’s any red flag. Don’t skip it just because the person is a child.
Sleep Problems: The Hidden Cost
If your child can’t fall asleep, or you’re waking up at 2 a.m. because your brain won’t shut off, stimulants might be why. Around 30 to 50% of people starting stimulant treatment report trouble sleeping. It’s not always the dose - it’s timing. Even extended-release formulas that last 10 to 12 hours can leave enough drug in the system to delay sleep onset.
The American Academy of Sleep Medicine found that stimulant users take, on average, 15 to 30 minutes longer to fall asleep than those on placebo. That might not sound like much, but when it happens every night, it piles up. Chronic sleep loss worsens ADHD symptoms - creating a vicious cycle: take more meds to focus better, sleep worse, feel worse the next day, take more meds.
Non-stimulants don’t always fix this. Atomoxetine can make you tired during the day. Guanfacine? It might actually help sleep. That’s why some doctors start with guanfacine for kids who struggle with both ADHD and insomnia. Melatonin (0.5 to 5 mg) taken 1 to 2 hours before bed can help reset the clock - but it doesn’t block the stimulant. It just helps the body know it’s time to wind down.
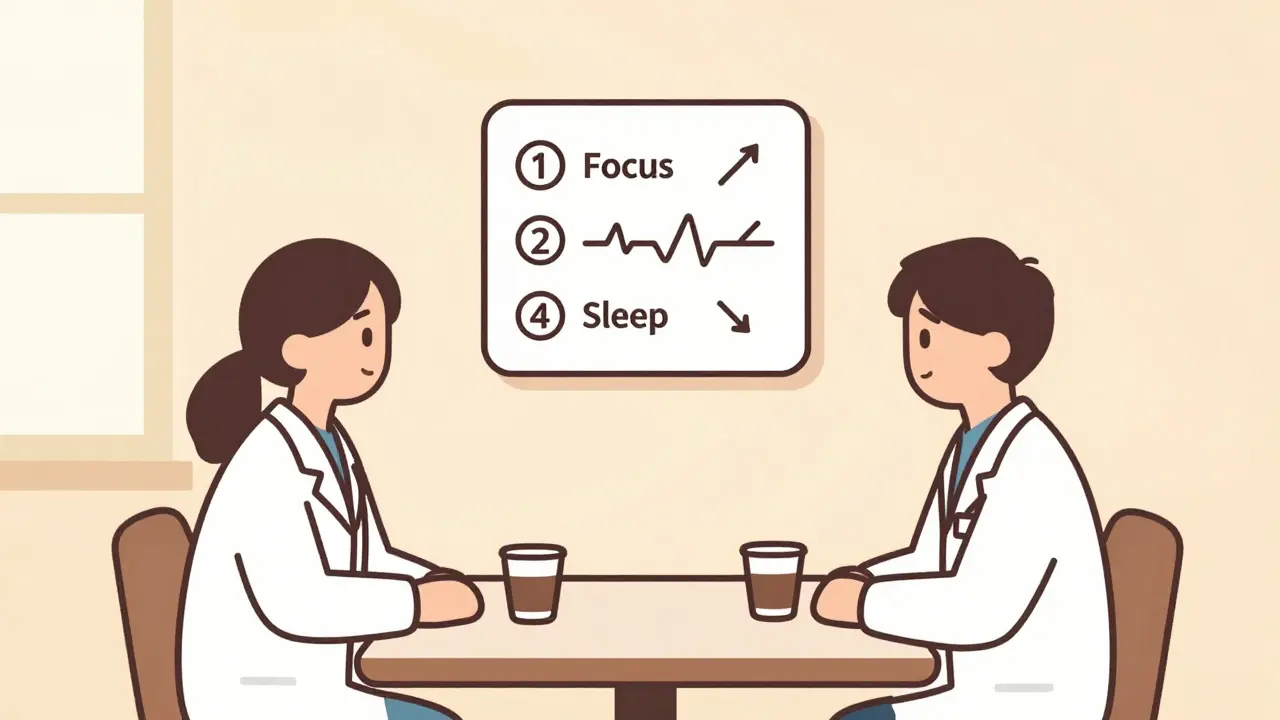
What Should You Do? Monitoring Is Key
Here’s the bottom line: you don’t need a heart scan before every prescription. The American Academy of Pediatrics and American Academy of Neurology agree: routine ECGs aren’t necessary for most people. But you do need to pay attention.
- Before starting: Get a baseline blood pressure and heart rate. Ask about family history - did anyone die suddenly before age 50? Any unexplained fainting?
- Three months in: Check again. Is the heart rate up? Is the BP climbing? A rise of more than 10 beats per minute or 10 mmHg systolic should trigger a conversation.
- Every 6 months: Keep checking. Even if things seem fine.
For high-risk patients - those with known heart disease, arrhythmias, or severe hypertension - a cardiologist should be part of the care team. For others, simple steps can reduce risk:
- Take the dose earlier in the day. No later than lunchtime for extended-release.
- Start low. A 5 mg dose of methylphenidate is often enough to start. Increase slowly.
- Consider switching. If sleep or heart rate stays high, try guanfacine or atomoxetine. They’re not magic, but they’re gentler on the system.
- Watch for symptoms: chest pain, palpitations, dizziness, fainting. Don’t ignore them.
The Bigger Picture: Risk vs. Reward
Let’s put the numbers in perspective. The JAMA Psychiatry study found that for every 1,000 people treated with ADHD stimulants over several years, maybe one or two would have a serious cardiovascular event. Meanwhile, untreated ADHD carries risks too - higher rates of accidents, job loss, substance abuse, depression, and even early death from injury or suicide.
Doctors aren’t ignoring the risks. The FDA now requires all new ADHD drugs to include long-term cardiovascular studies. The American Heart Association softened its early call for universal ECGs. Experts now agree: the benefits of these medications, for most people, still outweigh the risks.
But that doesn’t mean you treat everyone the same. A 12-year-old with mild ADHD and no family history? A low dose, careful monitoring, and a bedtime routine might be all you need. A 25-year-old with a history of high blood pressure and a cousin who died of sudden cardiac arrest? That’s a different conversation.
What matters isn’t fear. It’s awareness. It’s knowing what to watch for. It’s understanding that a medication that helps your child focus can also affect their heart rate - and that’s okay, as long as you’re watching.
What’s Next?
Research is moving fast. Scientists are building risk calculators that use age, dose, duration, and even genetic markers to predict who’s more likely to have side effects. Some clinics are already testing blood biomarkers to catch early signs of heart strain. In the next few years, personalized monitoring may become standard - not just for ADHD, but for all medications that affect the nervous system.
For now, the message is simple: don’t skip the checkups. Don’t ignore sleep problems. Don’t assume non-stimulants are safer - they’re not always. And don’t let fear stop treatment. But do stay informed. Stay curious. And stay in touch with your doctor.