Tacrolimus-Azole Interaction Dose Calculator
Dose Adjustment Tool
Why Mixing Azoles with Tacrolimus Can Be Deadly
If you’re on tacrolimus after a kidney, liver, or lung transplant, and your doctor prescribes an azole antifungal like voriconazole or posaconazole, you’re walking into a high-risk drug interaction. It’s not a rare edge case-it happens weekly in transplant clinics. Azoles don’t just treat fungal infections; they can cause your tacrolimus levels to spike 2 to 10 times higher than normal. That spike doesn’t just mean a lab result is off-it means your kidneys are under attack, your nerves might start tingling, and you could end up in the hospital with acute kidney injury.
This isn’t theoretical. A kidney transplant patient in Brisbane reported her tacrolimus levels jumped from 6.5 to 18.2 ng/mL in under 48 hours after starting voriconazole. Her creatinine doubled. She spent a week in the hospital. That’s not an outlier-it’s a textbook example of what happens when CYP3A4 inhibition meets immunosuppressant therapy.
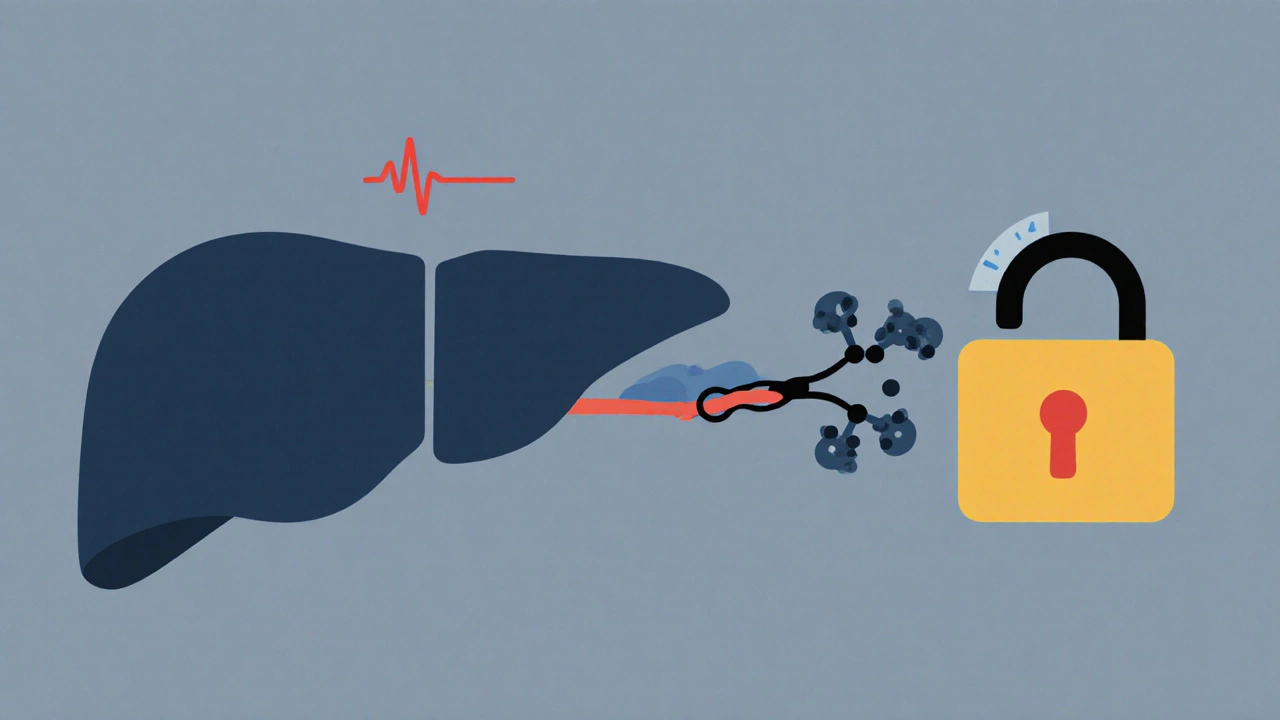
How Azoles Hijack Tacrolimus Metabolism
Tacrolimus doesn’t stay in your body long. About 95% of it gets broken down by enzymes in your liver-mainly CYP3A4 and CYP3A5. These enzymes act like molecular scissors, cutting tacrolimus into pieces your body can flush out. But azole antifungals? They’re not just passing through. They lock onto those same enzymes and shut them down.
Think of it like a traffic jam at a factory exit. Tacrolimus keeps being produced, but the exit gates are blocked. The drug piles up in your bloodstream. Ketoconazole is the strongest blocker-its inhibition constant (Ki) is as low as 0.002 μM. Voriconazole isn’t far behind. Even posaconazole, often seen as "safer," can still push tacrolimus levels up by 150-300%.
What’s worse? Tacrolimus has a narrow therapeutic window. The difference between a therapeutic level (5-10 ng/mL) and a toxic level (above 15 ng/mL) is small. A 200% increase doesn’t just nudge you into toxicity-it slams you into it.
The Kidney Takes the Brunt
Tacrolimus isn’t just toxic to your liver-it’s directly toxic to your kidneys. It causes vasoconstriction in the tiny blood vessels of the glomeruli, reducing blood flow. Over time, this leads to scarring, reduced filtration, and rising creatinine. When levels spike due to azoles, this damage accelerates.
Studies show that 15-20% of all tacrolimus-related kidney injury in transplant patients is directly tied to azole co-administration. In one 2020 retrospective analysis from Johns Hopkins, patients on voriconazole and tacrolimus had a 4.7 times higher risk of acute kidney injury compared to those on other antifungals.
And here’s the cruel twist: the damage often starts before you feel it. Creatinine rises slowly. You might feel fine, but your kidney function is already declining. By the time you’re dizzy or swollen, the injury may be partially irreversible.

Not All Azoles Are Created Equal
Some azoles are far worse than others. Here’s the real-world ranking based on interaction severity:
- Ketoconazole - Avoid entirely. Increases tacrolimus AUC by 300-500%. No safe dose exists without drastic reduction.
- Voriconazole - The most common culprit. Increases levels by 100-300%. Requires immediate dose reduction and daily monitoring.
- Itraconazole - Similar to voriconazole. Often used for aspergillosis, but just as dangerous.
- Posaconazole - Moderate interaction. Still raises levels by 150-250%. Requires 50-75% tacrolimus reduction.
- Isavuconazole - The outlier. Only increases levels by 30-50%. Often the preferred choice when available.
But here’s the catch: insurance often won’t cover isavuconazole as first-line. It’s more expensive. So clinicians are forced to use voriconazole or posaconazole-even though the risk is far higher.
What Transplant Teams Do to Stay Safe
Top transplant centers have protocols. They don’t guess. They don’t wait for creatinine to rise. They act before the spike happens.
Standard practice when starting an azole:
- Reduce tacrolimus dose by 50-75% for voriconazole, posaconazole, or itraconazole.
- Reduce by 75% or more for ketoconazole (if absolutely unavoidable).
- Check tacrolimus trough levels daily for the first 3-5 days.
- Then check 2-3 times weekly until stable.
- Hold the next dose if levels exceed 15 ng/mL, even if the patient feels fine.
One transplant pharmacy in Melbourne reduced nephrotoxicity events by 60% after implementing a standardized 75% dose reduction protocol for posaconazole. That’s not luck-it’s protocol.
Electronic alerts in EHR systems help, but they’re not foolproof. A 2022 study from UPMC found that 35% of severe toxicity cases happened because the alert was ignored or overridden. The real solution? Education and double-checks. Pharmacists must be involved in every antifungal order for transplant patients.
Alternatives That Don’t Trigger the Spike
If you need antifungal coverage but want to avoid this interaction, there are better options:
- Echinocandins (caspofungin, micafungin, anidulafungin): No CYP3A4 inhibition. Safe with tacrolimus. Used for invasive candidiasis.
- Lipid-formulation amphotericin B: Doesn’t inhibit CYP3A4, but carries its own nephrotoxicity risk. Use only if azoles and echinocandins aren’t options.
- Isavuconazole: Best azole alternative. Minimal interaction. If insurance allows, it’s the preferred choice.
Amphotericin B is tricky. It doesn’t interfere with tacrolimus metabolism, but it damages kidneys on its own. So combining it with tacrolimus? That’s stacking two nephrotoxins. Not ideal.
That’s why many centers now use echinocandins for candida and isavuconazole for aspergillosis-when possible. The goal isn’t just to treat the infection. It’s to do it without wrecking the transplant.
What’s Changing in 2025
The field is evolving. In 2023, the FDA approved a new extended-release tacrolimus formulation. It smooths out the peaks and valleys in blood levels, which may reduce nephrotoxicity-even during interactions.
Even more promising: genetic testing. About half of people of African descent and 10-15% of Caucasians have a gene variant (CYP3A5*1) that makes them fast metabolizers of tacrolimus. These patients naturally clear the drug faster. When they take azoles, their levels don’t spike as dramatically. But if you’re a slow metabolizer (CYP3A5*3/*3), you’re at much higher risk.
By 2024, the American Society of Transplantation is expected to recommend CYP3A5 genotyping before starting tacrolimus. It’s not routine yet-but it should be. Knowing your genotype could mean the difference between a safe antifungal course and a trip to the ICU.
What Patients Need to Know
If you’re on tacrolimus:
- Ask every doctor, "Is this medication going to affect my tacrolimus?" Even a simple antifungal cream can matter if it’s absorbed systemically.
- Know your latest tacrolimus level. Keep a log. Don’t assume your doctor remembers it.
- If you start a new antifungal and feel dizzy, nauseous, or notice less urine output, get your levels checked immediately.
- Don’t wait for symptoms. High levels can cause silent kidney damage.
Transplant survival rates are better than ever-97% at one year. But surviving the transplant isn’t enough. You have to survive the long-term risks too. This interaction kills more people than rejection in some centers.
Why This Interaction Keeps Happening
It’s not because doctors are careless. It’s because the system is broken.
Pharmacists are overloaded. EHR alerts are noisy. Insurance blocks better drugs. Patients are discharged with new prescriptions and no clear instructions. A 2022 survey of 127 transplant pharmacists found that 76% saw at least one unplanned hospital admission per month due to this interaction.
And here’s the silent truth: many transplant centers still don’t have a written protocol. They rely on memory, experience, or last-minute phone calls to the pharmacy. That’s not medicine. That’s gambling.
The solution isn’t more drugs. It’s better systems. Standardized order sets. Mandatory pharmacist review. Genetic testing. And above all-respecting the science. This interaction isn’t a myth. It’s a predictable, preventable disaster.
Can I take over-the-counter antifungals like clotrimazole with tacrolimus?
Topical clotrimazole or miconazole creams are generally safe because very little is absorbed into the bloodstream. But if you’re using oral antifungals-even fluconazole-or large amounts of topical products over broken skin, the risk increases. Always check with your transplant team before using any antifungal, even if it’s sold without a prescription.
How long does it take for tacrolimus levels to drop after stopping an azole?
It varies. Azoles stick around in your system for days to weeks. Voriconazole has a half-life of 6-12 hours, but its inhibitory effect on CYP3A4 can last 5-7 days after stopping. Tacrolimus levels may take up to 10-14 days to stabilize. Never increase your tacrolimus dose just because you stopped the azole. Keep monitoring for at least two weeks.
Is there a blood test to check if I’m at higher risk for this interaction?
Yes. A CYP3A5 genetic test can tell you if you’re a fast or slow metabolizer of tacrolimus. Fast metabolizers (CYP3A5 expressers) may tolerate higher doses and see smaller spikes with azoles. Slow metabolizers are at much higher risk. This test isn’t routine yet, but it’s becoming standard in major transplant centers. Ask your pharmacist or transplant coordinator.
Can I switch from tacrolimus to another immunosuppressant to avoid this?
Belatacept is an alternative that doesn’t rely on CYP3A metabolism, so it doesn’t interact with azoles. But it’s not right for everyone. It’s more expensive, requires IV infusions, and has a higher risk of early rejection in some patients. Most transplant centers still use tacrolimus as first-line because it’s more effective long-term. Switching isn’t a simple fix-it’s a complex decision made by your transplant team.
What signs should I watch for that mean my tacrolimus level is too high?
Early signs include tremors, headaches, tingling in hands or feet, high blood pressure, and reduced urine output. Later signs are swelling in legs, extreme fatigue, nausea, and confusion. But here’s the danger: many patients feel fine even with dangerously high levels. That’s why regular blood tests are non-negotiable. Don’t wait for symptoms. Test before you feel bad.





Javier Rain
November 22, 2025 AT 00:22Just had a patient on voriconazole spike to 22 ng/mL last week. Creatinine went from 1.2 to 3.8 in 72 hours. We dropped tacrolimus by 75% immediately and held the next dose. She’s stable now, but it was terrifying. This isn’t theoretical-it’s happening in real time, every day.
Richard Wöhrl
November 23, 2025 AT 07:02Agreed. I’ve been pushing for CYP3A5 genotyping at our center for years. Slow metabolizers are walking time bombs if you give them voriconazole without adjusting. We finally got it approved last quarter. Now we test before starting tacrolimus at all. Game changer.
Vivian C Martinez
November 25, 2025 AT 04:10Isavuconazole is the quiet hero here. We switched three patients from voriconazole to isavuconazole last month. All had stable tacrolimus levels within 48 hours. No ICU visits. No creatinine spikes. It’s not perfect, but it’s the safest azole we’ve got.
Karla Morales
November 25, 2025 AT 19:07Let’s be real-this isn’t about science. It’s about $$$.
Isavuconazole costs $4,000 a course. Voriconazole? $400.
Insurance won’t cover the better drug unless you fight for 3 weeks. So we use the dangerous one. The system is broken, not the doctors.
Laurie Sala
November 26, 2025 AT 00:05I lost my cousin to this. He was 42. Had a liver transplant. Got a yeast infection. They gave him posaconazole. Said it was "safe." His kidneys failed. He died waiting for a new one. Nobody warned us. Nobody checked his levels. This is murder by protocol.
Pramod Kumar
November 27, 2025 AT 14:56My uncle’s a transplant patient in Delhi. He got a fungal rash. Local doctor gave him oral fluconazole. He didn’t tell his transplant team. His tacrolimus level jumped. He ended up in ICU. Took 6 months to recover. Never again. Always ask. Always double-check. No exceptions.
Manjistha Roy
November 28, 2025 AT 07:00Topical clotrimazole is fine, but I once saw a nurse apply it to a 20cm wound on a transplant patient’s leg. Three days later, tacrolimus spiked. Turns out, broken skin absorbs more than you think. Always check the route. Always.
Brandy Walley
November 29, 2025 AT 19:23Charmaine Barcelon
November 29, 2025 AT 19:54You’re lucky you didn’t die. That’s not adaptation-that’s negligence. People who say this are the same ones who say "vaccines cause autism." This isn’t opinion. It’s pharmacology. And you’re putting lives at risk.
Katy Bell
November 29, 2025 AT 22:23I’m a nurse in a transplant unit. We had a patient who didn’t feel a thing until her creatinine hit 5.2. No tremors. No tingling. Just… quiet kidney failure. That’s why we test even when they feel fine. Silence kills here.
Suresh Ramaiyan
December 1, 2025 AT 02:54It’s funny how we treat drugs like they’re magic bullets. We forget they’re chemicals that talk to each other in ways we barely understand. Tacrolimus and azoles? They’re like two people in a crowded room-one shouting, one blocking the exits. No one’s at fault. But someone’s got to open the door.
Ragini Sharma
December 1, 2025 AT 20:27Linda Rosie
December 2, 2025 AT 10:11shreyas yashas
December 3, 2025 AT 03:11My cousin’s a transplant doc in Mumbai. He told me they started a daily tacrolimus check list after three patients crashed last year. Now they use a simple whiteboard: Azole? Yes/No. Level? ______. Next check? ______. No fancy tech. Just discipline. It works.