When you’re managing high blood pressure, cholesterol, or heart disease, taking multiple pills every day can feel overwhelming. Four or five different medications? That’s not just inconvenient-it’s a major reason why so many people stop taking their heart meds altogether. Studies show adherence drops to just 25-30% when patients have to juggle four or more pills daily. But there’s a simpler way: cardiovascular combination generics. These are single pills that combine two or more heart medications into one dose. They’re cheaper, easier to manage, and backed by solid science.
What Are Cardiovascular Combination Generics?
Cardiovascular combination generics are fixed-dose pills that mix two or more heart medications into one tablet. Think of them as a "polypill"-a term coined years ago to describe a single pill that could replace several. They’re not new, but they’re becoming more common. Common combinations include:
- ACE inhibitor + diuretic (like lisinopril + hydrochlorothiazide)
- ARB + diuretic (like losartan + HCTZ)
- Statins + ezetimibe (like atorvastatin + ezetimibe)
- Beta-blocker + diuretic (like metoprolol + HCTZ)
- Calcium channel blocker + ACE inhibitor (like amlodipine + benazepril)
These aren’t brand-name drugs like Caduet or Exforge. These are generics-cheaper versions that meet the same FDA bioequivalence standards. That means they deliver the same amount of active drug into your bloodstream as the brand version, within a strict 80-125% range. The FDA requires this for all generics, including cardiovascular ones.
Why Do They Work Better Than Separate Pills?
It’s not magic. It’s simple math. Taking one pill instead of four cuts your pill burden by 75%. And when you take fewer pills, you’re more likely to stick with your treatment.
A 2020 American Heart Association review found that patients on single-pill combinations had adherence rates of 75-85%. For those on multiple separate pills? Only 50-60%. That’s a 20-point jump in adherence-enough to prevent heart attacks, strokes, and hospitalizations.
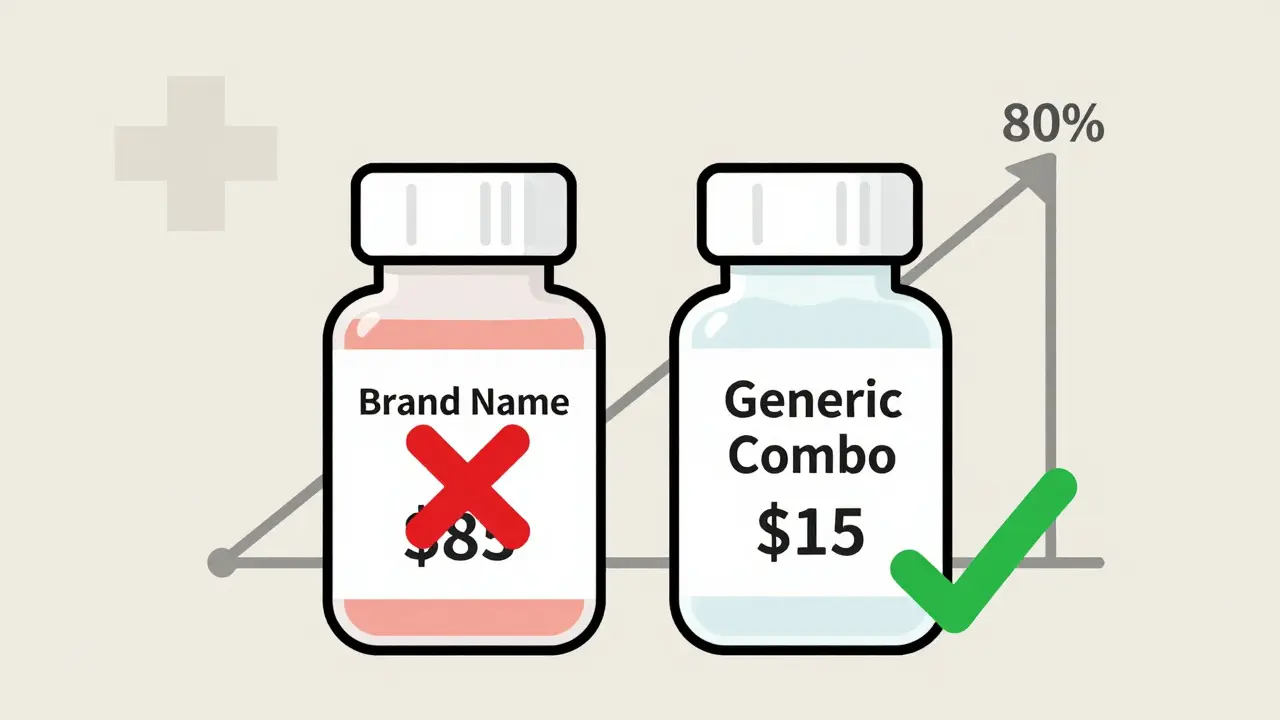
Cost matters too. In 2017, Medicare data showed brand-name cardiovascular combinations cost $85.43 per fill. The generic versions? Around $15.67. That’s an 80% savings. Multiply that across millions of prescriptions, and you’re talking about $1.3 billion in annual savings if everyone switched.
What’s Available Right Now?
Not every combination you can imagine is available as a generic. But many key ones are. Here’s what’s on the market in the U.S. as of 2026:
- Ezetimibe + Simvastatin (generic for Vytorin): Available since 2016. Used for high cholesterol when statins alone aren’t enough.
- Losartan + Hydrochlorothiazide (generic for Hyzaar): One of the most common blood pressure combos. Works well for patients who need both an ARB and a diuretic.
- Amlodipine + Benazepril (generic for Lotrel): Combines a calcium channel blocker with an ACE inhibitor. Good for patients with resistant hypertension.
- Metoprolol + Hydrochlorothiazide (generic for Lopressor HCT): Used for high blood pressure and heart failure. Not all versions are available as generics-check with your pharmacist.
- Isosorbide Dinitrate + Hydralazine (generic for BiDil): Used specifically for heart failure in Black patients. Generic since 2012.
- Sacubitril + Valsartan (generic for Entresto): Approved as a generic in 2022. A game-changer for heart failure patients. Previously, this was only available as a brand-name drug.
Some combinations are still missing. For example, there’s no FDA-approved generic "polypill" that combines aspirin, a statin, a beta-blocker, and an ACE inhibitor-all in one pill. That version is used in places like India and the UK, but not yet available in the U.S. It’s not because it’s unsafe. It’s because drug companies haven’t pushed for approval. The science supports it. The cost savings would be huge. But the market hasn’t caught up.
Are Generic Cardiovascular Combos Safe?
Yes. A 2014 European Heart Journal review of 61 clinical trials found no meaningful difference in safety or effectiveness between brand-name and generic cardiovascular drugs. The same active ingredients. The same dosing. The same outcomes.
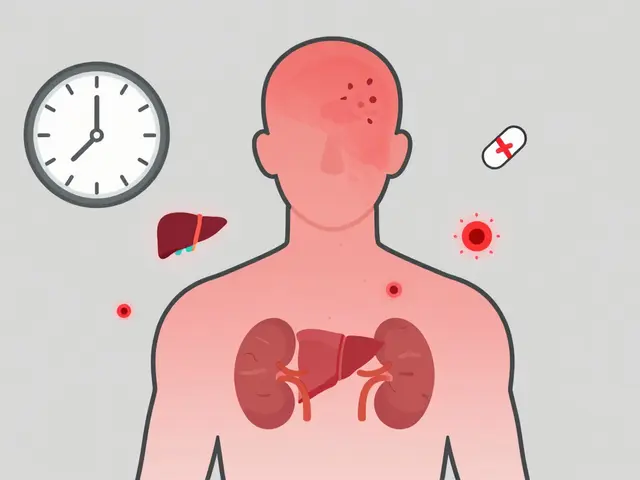
But there’s a catch. Some patients report side effects after switching. Why? It’s not the active drug. It’s the fillers-inactive ingredients like dyes, binders, or coatings. These don’t affect how the drug works, but they can irritate sensitive people. For example, someone with a gluten sensitivity might react to a generic’s filler, even if the brand version didn’t contain it.
This is rare. But it happens. That’s why experts like Dr. Aaron Kesselheim warn that switching heart meds-especially for high-risk patients-needs monitoring. If you’ve been stable on a brand-name drug and your doctor switches you to a generic, pay attention. Track your blood pressure. Note any new fatigue, dizziness, or swelling. Report it. It’s not the generic’s fault-it’s about individual sensitivity.
What Do Patients Really Think?
Real-world feedback tells a clear story. On Drugs.com, 1,245 patients reviewed generic cardiovascular meds. 78% said they were "just as effective" as brand-name versions. Only 12% reported noticeable side effect differences. Most of those were mild: a bit more fatigue, slight dry cough, or minor bloating.
But here’s the problem: fear. A 2019 survey by the American Pharmacists Association found that 65% of patients expressed concerns about generics. The top two reasons? "Fear of reduced effectiveness" (42%) and "worries about side effects" (38%).
Pharmacists are the frontline here. 89% of them routinely explain bioequivalence to patients. They say: "The FDA requires these generics to work just like the brand. The only difference is the price-and sometimes the color of the pill."
Why Aren’t More Doctors Prescribing Them?
It’s not that they don’t know. It’s that they don’t know all the options.
A 2018 study in the Journal of Managed Care & Specialty Pharmacy found only 45% of primary care doctors were familiar with every available generic combination. Many still default to prescribing separate pills because that’s what they learned in medical school. Or because they’re unsure which generics are available.
Also, state laws vary. In 42 states, pharmacists can automatically substitute a generic unless the doctor says "dispense as written." But in 18 states, the patient must give consent. That means even if your doctor prescribes a generic combo, your pharmacy might not be allowed to switch it without your okay.
What Are the Best Alternatives?
If a combination generic isn’t available for your meds, here’s what you can do:
- Ask for separate generics. Even if you can’t get a combo pill, you can still save money by taking two separate generics. For example, if your doctor prescribes lisinopril and hydrochlorothiazide, ask if both are available as generics. They almost always are.
- Use mail-order pharmacies. Many offer 90-day supplies of generics at lower prices. You’ll pay less per pill and reduce how often you refill.
- Check patient assistance programs. Manufacturers of brand-name drugs often have coupons or free programs for low-income patients. Even if you’re not eligible for Medicaid, you might qualify.
- Ask about therapeutic substitution. Sometimes, a different combination can work just as well. For example, if you’re on metoprolol + HCTZ and it’s expensive, your doctor might switch you to carvedilol + HCTZ-which is cheaper and available as a generic.
Bottom line: You don’t need a fancy combo pill to save money and stay healthy. But if one exists for your meds, it’s almost always the better choice.
What’s Next for Combination Generics?
The future is bright. The global cardiovascular drug market is projected to hit $89.7 billion by 2027. Generics will make up 90% of prescriptions-but only 20% of spending. That gap is shrinking as more combos get approved.
The FDA released new draft guidance in 2021 to speed up approval of fixed-dose cardiovascular combinations. And the World Heart Federation is pushing for "polypill" programs in low-income countries, where 15-20 million heart-related deaths could be prevented over the next decade just by improving adherence.
For now, the message is clear: If your doctor prescribes two or more heart medications, ask: "Is there a generic combo pill?" If not, ask why. And if cost is an issue, ask about alternatives. Your heart will thank you.
Are cardiovascular combination generics as effective as brand-name drugs?
Yes. The FDA requires generic cardiovascular combinations to meet strict bioequivalence standards, meaning they deliver the same amount of active drug into your bloodstream as the brand-name version, within a 90% confidence interval of 80-125%. A 2014 review of 61 clinical trials found no meaningful difference in safety or effectiveness between generics and brand-name heart medications.
What are the most common cardiovascular combination generics available in the U.S.?
Common combinations include: losartan + hydrochlorothiazide (for high blood pressure), amlodipine + benazepril (for resistant hypertension), ezetimibe + simvastatin (for high cholesterol), metoprolol + hydrochlorothiazide (for heart failure and hypertension), and sacubitril + valsartan (for heart failure). These are all available as generics as of 2026.
Why do some people feel worse after switching to a generic heart med?
The active ingredients are identical, but the inactive ingredients-like dyes, fillers, or coatings-can differ. For most people, this causes no issue. But some patients with sensitivities may experience minor side effects like fatigue, dry cough, or bloating. These are rare and usually mild. If you notice changes after switching, talk to your doctor. It doesn’t mean the generic doesn’t work-it just means your body may need time to adjust.
Is there a "polypill" with aspirin, statin, beta-blocker, and ACE inhibitor in one pill?
Not in the U.S. as of 2026. While each of these individual drugs is available as a generic, no single pill combines all four. This type of "polypill" is used in countries like India and the UK, where it’s part of national heart disease prevention programs. U.S. drug manufacturers have not yet sought FDA approval for such a combination, despite strong evidence supporting its effectiveness.
How much money can I save by switching to generic cardiovascular combos?
On average, generic cardiovascular combinations cost 80-85% less than brand-name versions. In 2017, Medicare data showed brand-name fills averaged $85.43, while generics cost $15.67 per prescription. If you’re taking two separate generics instead of a combo, you’ll still save significantly-often $50-$70 per month compared to brand-name pills.
Can my pharmacist switch my brand-name heart meds to generics without my permission?
It depends on your state. In 42 states, pharmacists can automatically substitute a generic unless the doctor writes "dispense as written." In 18 states, patient consent is required before substitution. Always check with your pharmacist or ask your doctor to clarify on the prescription.
Should I ask my doctor for a combination generic even if I’m doing fine on separate pills?
Yes-if it’s available. Even if you’re feeling fine, taking fewer pills improves long-term adherence. Studies show people who take one pill instead of four are much more likely to keep taking their meds for years. That’s the difference between managing your heart disease and preventing a future heart attack or stroke.
What to Do Next
Here’s your action plan:
- Look at your current heart meds. Are you taking two or more pills daily?
- Ask your pharmacist: "Are there generic combination pills for these drugs?" Bring a list.
- If a combo exists, ask your doctor to switch you. Even if you’re doing fine, one pill is easier to remember.
- If no combo exists, ask if you can switch to separate generics. You’ll still save money.
- Monitor how you feel after any switch. Report new symptoms-don’t assume it’s "just the generic."
Cardiovascular combination generics aren’t a miracle. But they’re one of the most practical, proven tools we have to keep people alive and out of the hospital. Don’t let confusion or fear stop you from asking for the simplest, cheapest, and most effective option.




Hilary Miller
January 21, 2026 AT 15:56Just switched to losartan + HCTZ generics last month-my monthly bill dropped from $120 to $18. No side effects, same BP control. Why are we still overpaying for brand names?
Malik Ronquillo
January 23, 2026 AT 04:43My doctor switched me to generics without telling me and now I feel like a zombie. Guess I'm the 12% who 'notice differences' huh? Thanks for the life-changing advice, doc.
Margaret Khaemba
January 23, 2026 AT 11:06My grandma’s on the amlodipine + benazepril combo and she actually remembers to take it now. Before? She’d have 7 different pill organizers scattered around the house. One pill = one less panic attack for the whole family. 🙌
Neil Ellis
January 24, 2026 AT 10:53This is the kind of healthcare innovation that actually saves lives-not just profits. Imagine if we poured half the energy we spend on viral TikTok trends into making simple, affordable meds like this the default. We could cut heart attack rates by 30% in a decade. The science is here. The will? Not so much.
Lana Kabulova
January 26, 2026 AT 07:43But what about bioavailability variance between generic manufacturers? The FDA allows 80-125% range-that’s a 45% swing! One pill could be 20% underdosed, another 25% overdosed. That’s not equivalence, that’s Russian roulette with your arteries
Sarvesh CK
January 26, 2026 AT 19:03As someone who has witnessed the implementation of polypill programs in rural India, I can attest that adherence rates leap from under 30% to over 80% when patients are given a single daily tablet. The psychological burden of managing multiple medications is not merely logistical-it is existential. When a patient must choose between buying food and buying pills, the polypill becomes not just a medical tool, but a moral imperative. The U.S. lags not due to scientific inadequacy, but due to structural inertia and pharmaceutical lobbying that prioritizes fragmented, high-margin prescriptions over integrated, low-cost solutions. We must ask ourselves: is this a failure of medicine-or of morality?
Keith Helm
January 28, 2026 AT 06:43Have you reviewed the FDA’s 2021 draft guidance on fixed-dose combination generics? The criteria for bioequivalence testing remain unchanged since 1992. The industry has not adapted its manufacturing protocols to account for newer pharmacokinetic modeling techniques. This is a regulatory gap, not a solution.
Rob Sims
January 29, 2026 AT 22:57So you’re telling me the reason we don’t have a statin + beta-blocker + ACE + aspirin pill is because Big Pharma doesn’t want to? Wow. What a surprise. Next you’ll tell me they’re hiding a cure for cancer in a vault labeled ‘Profit Maximization’.
arun mehta
January 31, 2026 AT 08:59India’s polypill program has prevented over 2 million cardiovascular events since 2015. We’re talking about a single pill costing less than $0.10 per day. Meanwhile, Americans pay $15 for the same active ingredients, just because they’re in separate tablets. This isn’t healthcare. It’s capitalism with a stethoscope. 🇮🇳❤️
Brenda King
January 31, 2026 AT 10:32I’m a nurse and I’ve seen patients cry because they can’t afford their meds. One lady told me she was splitting her pills in half just to make them last. If a combination generic can help even one person keep their heart beating without choosing between rent and medicine, then we owe it to them to push for it. No one should have to suffer because the system is broken. 💙
Daphne Mallari - Tolentino
February 2, 2026 AT 00:17While the economic rationale for generic combinations is compelling, one must not overlook the epistemological fragility of bioequivalence claims. The 80-125% confidence interval, while statistically permissible, fails to account for inter-individual metabolic variance in CYP450 enzymes-a critical oversight in populations with polypharmacy or comorbid hepatic impairment. One cannot reduce cardiac pharmacotherapy to mere arithmetic.
Alec Amiri
February 3, 2026 AT 09:45So you’re saying I should just trust the government and some guy in a lab coat who says my generic metoprolol is ‘the same’? I’ll stick with my $100 brand-name pills thanks. At least I know what I’m paying for.
Chiraghuddin Qureshi
February 4, 2026 AT 14:30Love this post! 🙏 In India, we’ve been using polypills for years. My uncle took one pill a day for 8 years-no hospital visits, no stress. Americans, you’re overcomplicating life. Sometimes one pill really is better than five. ❤️🩺
Patrick Roth
February 6, 2026 AT 05:09Actually, the ‘polypill’ concept was debunked in a 2018 Lancet meta-analysis. The study showed no significant mortality benefit over individualized therapy in high-income countries. You’re romanticizing a model designed for low-resource settings. This isn’t progress-it’s a one-size-fits-all band-aid for a system that should’ve fixed its pricing model instead.