When you can’t sleep because your nose is stuffed up or your mind won’t shut off, doxylamine succinate often shows up as a go-to solution. It’s in many over-the-counter sleep aids and cold medicines. But is it the best choice? And what happens if it doesn’t work-or gives you that groggy, hungover feeling the next day? You’re not alone in wondering if there’s something better.
What is doxylamine succinate?
Doxylamine succinate is a first-generation antihistamine. It blocks histamine in the brain, which is why it makes you drowsy. That’s also why it’s used for allergies-it reduces runny nose, sneezing, and itchy eyes. But its strongest use? Short-term sleep help.
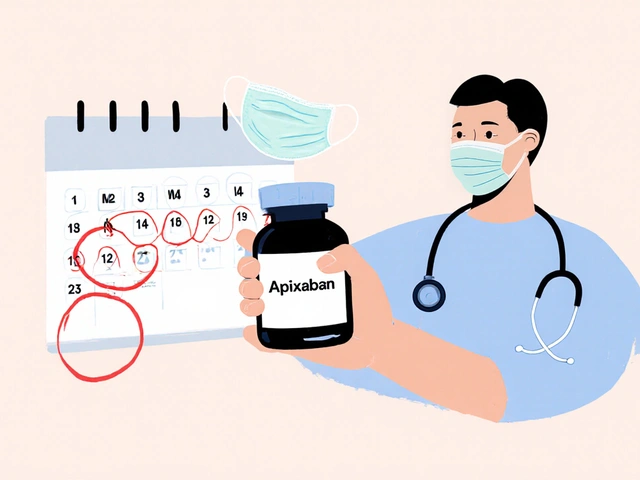
It’s the main ingredient in Unisom SleepTabs, and it’s often combined with pain relievers in nighttime cold formulas. The typical dose is 25 mg taken 30 minutes before bed. Most people feel sleepy within 20 to 30 minutes. Effects last 6 to 8 hours. But here’s the catch: it doesn’t just help you fall asleep. It changes your sleep architecture. You spend more time in light sleep and less in deep, restorative stages. That’s why you might wake up feeling off, even after 8 hours.
It’s not addictive like benzodiazepines, but your body can build tolerance. After a few weeks of regular use, you might need more to get the same effect. And if you stop suddenly, rebound insomnia is common.
Why look for alternatives?
Many people try doxylamine because it’s cheap, easy to find, and seems to work at first. But after a few nights, side effects pile up: dry mouth, blurred vision, constipation, next-day drowsiness, and sometimes confusion or dizziness-especially in older adults.
Studies from the Journal of Clinical Sleep Medicine show that first-gen antihistamines like doxylamine don’t improve sleep quality long-term. They just mask symptoms. And for people over 65, the American Geriatrics Society lists doxylamine as a medication to avoid because of the risk of falls and cognitive decline.
If you’ve been using it for more than two weeks, it’s time to consider alternatives. Not because doxylamine is dangerous-it’s not-but because better options exist that don’t mess with your brain chemistry as much.
Melatonin: The natural sleep regulator
Melatonin is your body’s own sleep hormone. It rises at night and tells your brain it’s time to rest. Supplementing with melatonin doesn’t force sleep-it just helps reset your internal clock.
It’s ideal if your sleep problems come from jet lag, shift work, or irregular schedules. Doses range from 0.5 mg to 5 mg. Lower doses often work just as well as higher ones, and they’re less likely to cause grogginess.
Compared to doxylamine, melatonin doesn’t cause dry mouth, urinary retention, or next-day fog. It’s safe for long-term use in most people. The downside? It doesn’t work well for people with anxiety-driven insomnia or chronic pain. It’s not a sedative. It’s a signal.
One 2023 meta-analysis in Sleep Medicine Reviews found melatonin helped people fall asleep 7 minutes faster on average and increased total sleep time by about 13 minutes. Small gains-but sustainable, without side effects.
Diphenhydramine: The other OTC sleep aid
Diphenhydramine is in Benadryl and many nighttime sleep aids. Like doxylamine, it’s a first-gen antihistamine. So why compare them?
They’re very similar. Both cause drowsiness, dry mouth, and next-day grogginess. But doxylamine lasts longer-up to 8 hours-while diphenhydramine wears off in 4 to 6. That means diphenhydramine might be better if you wake up too early and want to fall back asleep without feeling hungover.
But here’s the real difference: doxylamine is slightly more potent. A 25 mg dose of doxylamine has a stronger sedative effect than a 50 mg dose of diphenhydramine. That also means the side effects are more likely to be intense.
Neither is recommended for long-term use. Both can impair memory and motor skills in older adults. And if you’re taking other medications-especially antidepressants or blood pressure drugs-both can interact dangerously.

Zolpidem (Ambien): Prescription, but not always better
If OTC options fail, doctors sometimes prescribe zolpidem. It’s a non-benzodiazepine sleep medication that targets specific receptors in the brain to induce sleep.
Zolpidem works faster than doxylamine-often within 15 minutes. It’s more effective for people with severe insomnia. But it comes with risks: sleepwalking, memory loss, dependency, and even complex behaviors like driving while asleep.
Unlike doxylamine, zolpidem doesn’t cause dry mouth or constipation. But it can cause strange dreams, nausea, and a metallic taste. It’s also more expensive and requires a prescription.
It’s not a long-term fix. The FDA recommends using it for no more than 7 to 10 days. For most people, it’s a bridge-not a solution.
Cognitive Behavioral Therapy for Insomnia (CBT-I): The gold standard
If you’ve tried pills and they didn’t stick, CBT-I might be the answer you didn’t know you needed.
It’s not a drug. It’s a structured program that teaches you how to change thoughts and habits that keep you awake. Techniques include sleep restriction, stimulus control, relaxation training, and cognitive restructuring.
A 2024 study in The Lancet followed 1,200 adults with chronic insomnia. Those who did CBT-I improved sleep quality more than those taking doxylamine, zolpidem, or melatonin. And the benefits lasted a year after treatment ended.
CBT-I doesn’t work overnight. It takes 4 to 8 weeks. But unlike pills, it doesn’t wear off. It rewires your brain’s relationship with sleep.
Many online programs now offer CBT-I for under $100. Some insurance plans cover it. It’s the only sleep treatment the American College of Physicians recommends as first-line for chronic insomnia.
Other natural options: Magnesium, valerian, and chamomile
Some people turn to herbal or supplement-based options.
- Magnesium glycinate helps relax muscles and calm the nervous system. Doses of 200-400 mg at night may improve sleep onset and reduce nighttime waking.
- Valerian root has been used for centuries. Some studies show it can reduce time to fall asleep, but results are mixed. It can smell unpleasant and cause headaches in some.
- Chamomile tea is gentle. The apigenin in chamomile binds to GABA receptors, similar to anti-anxiety drugs-but much milder. A cup 30 minutes before bed can be a soothing ritual.
None of these are as fast-acting as doxylamine. But they’re safer, especially for long-term use. They’re best for mild sleep issues or as part of a bedtime routine.
Which alternative is right for you?
There’s no one-size-fits-all. Your choice depends on why you can’t sleep.
| Option | Speed of Action | Duration | Next-Day Drowsiness | Long-Term Safety | Best For |
|---|---|---|---|---|---|
| Doxylamine Succinate | 20-30 min | 6-8 hours | High | Poor (tolerance, cognitive risk) | Short-term, severe insomnia |
| Melatonin | 30-60 min | 4-6 hours | Low | Good | Jet lag, circadian rhythm issues |
| Diphenhydramine | 20-40 min | 4-6 hours | Medium | Poor | Occasional use, shorter sleep windows |
| Zolpidem | 10-20 min | 6-8 hours | Medium | Risky (dependency) | Severe insomnia (short-term only) |
| CBT-I | Weeks | Long-lasting | None | Excellent | Chronic insomnia |
| Magnesium | 60-90 min | Variable | Very low | Excellent | Mild sleep issues, muscle tension |
If you’re young and just need help falling asleep once in a while, doxylamine might be fine. But if you’re over 50, have anxiety, or have been using it for more than a month, switch.
Melatonin is the safest starting point for most. CBT-I is the most effective long-term solution. And if you’re stuck, talk to a doctor-don’t just keep reaching for the same bottle.
When to stop doxylamine
Stop using doxylamine if:
- You’ve used it for more than 2 weeks
- You feel groggy, dizzy, or confused during the day
- You’re over 65
- You’re taking other sedatives, antidepressants, or anticholinergic drugs
- You’ve noticed memory lapses or trouble concentrating
Don’t quit cold turkey. Reduce the dose slowly-say, take it every other night for a week, then every third night. That helps avoid rebound insomnia.
Replace it with something better: a consistent bedtime, a warm bath, dim lights, and maybe a magnesium supplement. Sleep isn’t something you take-it’s something you build.
Is doxylamine succinate the same as Benadryl?
No. Doxylamine succinate is in Unisom SleepTabs, while Benadryl contains diphenhydramine. Both are first-gen antihistamines and cause drowsiness, but doxylamine is stronger and lasts longer. They’re similar, but not interchangeable.
Can I take doxylamine every night?
No. Taking it nightly can lead to tolerance, next-day drowsiness, and cognitive issues-especially in older adults. It’s meant for occasional, short-term use only. If you need sleep help every night, see a doctor about underlying causes like sleep apnea or anxiety.
Does melatonin work better than doxylamine?
For falling asleep faster, doxylamine works quicker. But melatonin is safer for long-term use and doesn’t cause grogginess or disrupt deep sleep. Melatonin is better for circadian rhythm issues; doxylamine is a sedative. They serve different purposes.
What’s the safest sleep aid for seniors?
The American Geriatrics Society advises against doxylamine, diphenhydramine, and similar antihistamines for older adults due to fall and dementia risks. Melatonin (low dose, 0.5-1 mg) or CBT-I are safer options. Always talk to a doctor before starting any new sleep aid.
Can doxylamine help with allergies?
Yes. Doxylamine blocks histamine, which reduces allergy symptoms like sneezing and runny nose. But because it causes drowsiness, it’s not ideal for daytime use. Second-gen antihistamines like loratadine or cetirizine are better for allergies during the day-they don’t make you sleepy.
Next steps: What to do now
Stop reaching for the same bottle every night. Ask yourself: Why am I sleeping poorly?
Keep a sleep diary for a week. Note when you go to bed, how long it takes to fall asleep, how many times you wake up, and how you feel in the morning. That data helps you-and a doctor-see patterns.
If you’re using doxylamine for allergies, switch to a non-drowsy option like loratadine during the day. If it’s insomnia, try melatonin for 2 weeks. If that doesn’t help, look into a CBT-I program. Many are available online through apps like Sleepio or CBT-I Coach.
Sleep isn’t a problem you fix with a pill. It’s a habit you rebuild. Start small. Be patient. Your body will thank you.





Mariam Kamish
October 28, 2025 AT 03:01Doxxylamine? More like dox-sleep-and-regret-later 😴💊
Emma Hanna
October 28, 2025 AT 15:16Let me be perfectly clear: using doxylamine every night is not just irresponsible-it’s a slow-motion assault on your prefrontal cortex!!
You think you’re 'just sleeping'-but you’re actually training your brain to forget how to rest naturally!!
And don’t even get me started on the dry mouth, the blurred vision, the cognitive fog that lingers like a bad hangover from a college binge!!
This isn’t medicine-it’s chemical surrender!!
liam coughlan
October 29, 2025 AT 16:03CBT-I changed my life. No pills. No grogginess. Just better sleep habits.
Took 6 weeks. Worth every minute.
Dirk Bradley
October 30, 2025 AT 03:59One must acknowledge that the pharmacological landscape of sleep aids is, in many respects, a reflection of our cultural aversion to discomfort and our pathological obsession with pharmacological quick fixes.
While melatonin offers a neurochemically benign alternative, its efficacy remains statistically marginal-7 minutes faster? That’s not sleep hygiene; that’s a placebo with a vitamin label.
CBT-I, by contrast, represents the only evidence-based, neuroplasticity-driven intervention that genuinely reconfigures the sleep-wake architecture-not merely sedates it.
It is, quite frankly, the only approach worthy of the term 'treatment.' The rest? Symptom management masquerading as solutions.
And let us not overlook the alarming normalization of anticholinergic burden in the elderly-a demographic that should be protected, not poisoned with OTC sedatives that increase dementia risk by 50% in longitudinal studies.
One wonders whether the FDA’s passive stance on these agents reflects regulatory capture or a collective societal denial of the cost of convenience.
For those who dismiss CBT-I as 'too slow,' one might ask: what is the alternative? A lifetime of pharmacological dependency? A gradual erosion of executive function?
There is no ethical justification for perpetuating the myth that a pill can substitute for behavioral recalibration.
And yet, here we are: millions consuming doxylamine like candy, while sleep specialists plead into the void.
It’s not just poor sleep-it’s a public health failure dressed in 25mg capsules.
Perhaps the real question isn't 'what works best?'-but 'why do we refuse to do the work?'
Brian O
October 31, 2025 AT 21:32I used to take Unisom every night for years. Felt fine until I started forgetting where I put my keys… then my phone… then my wife’s birthday.
Switched to melatonin (1mg) + CBT-I app. No more fog. No more panic when I wake up at 3am.
Still wake up sometimes-but now I just breathe. No pills needed.
Don’t let anyone tell you sleep is a problem you fix with chemicals.
Shawn Baumgartner
November 2, 2025 AT 19:58Let’s be real: doxylamine is just Big Pharma’s way of keeping the masses docile while they profit off the insomnia industrial complex.
They don’t want you to fix your sleep-they want you to buy their pills forever.
CBT-I? Too expensive. Too slow. Too much effort.
So they sell you 25mg of chemical sedation and call it 'help.'
Meanwhile, your hippocampus is slowly turning to mush.
And the FDA? They’re asleep at the wheel.
Wake up. Stop being a zombie.
Cassaundra Pettigrew
November 3, 2025 AT 06:13AMERICA NEEDS TO STOP TAKING SLEEP PILLS LIKE THEY’RE CANDY!!
THIS ISN’T CANADA. THIS ISN’T SWEDEN. WE’RE NOT HERE TO BE QUIET, GROGGY, BRAIN-ROTTED ZOMBIES!!
IF YOU CAN’T SLEEP WITHOUT A DRUG, YOU’RE NOT SICK-YOU’RE WEAK!!
GET UP. GO FOR A WALK. TURN OFF THE PHONE. STOP BEING A COWARD!!
THEY WANT YOU DEPRESSED. THEY WANT YOU DROWSY. THEY WANT YOU TO BUY MORE PILLS!!
STOP BEING A SHEEP!!
Manish Pandya
November 4, 2025 AT 23:33I’ve been using 0.5mg melatonin for 8 months now. No side effects. No grogginess. Just better rhythm.
Also started reading before bed-no screens. Changed everything.
People think sleep is about pills. It’s about routine.
Simple stuff works if you stick with it.
Navin Kumar Ramalingam
November 5, 2025 AT 19:02CBT-I is the only real solution, but who has time for that? You gotta eat, pay bills, scroll TikTok.
So yeah, I take Unisom. It’s not ideal, but it’s what keeps me functional.
And honestly? I’d rather be groggy than exhausted.
Real talk: society doesn’t care if you sleep. It just wants you productive.
So we take the pill.
And we call it 'survival.'
Gary Katzen
November 7, 2025 AT 14:42I’ve been on doxylamine for 3 months. Started feeling off-headaches, dry mouth, weird dreams.
Went cold turkey. Woke up every hour for a week.
Now I’m tapering: every other night, then every third.
Added magnesium glycinate. Feels better already.
Thanks for the warning, OP.
James Gonzales-Meisler
November 8, 2025 AT 02:45Did you know that doxylamine’s half-life is 10–12 hours in elderly patients? That’s not a sleep aid-it’s a 12-hour chemical restraint.
And yet, it’s sold over the counter like aspirin.
There’s no regulatory oversight. No mandatory warnings. No FDA-mandated black box for cognitive decline.
This isn’t an oversight.
This is negligence.
Steve Harvey
November 8, 2025 AT 04:54They don’t want you to know this, but doxylamine is linked to the rise in Alzheimer’s cases since 2010.
The CDC knows. The FDA knows.
But the pharmaceutical lobby owns Congress.
They’re slowly turning us into walking zombies so we don’t question the system.
Check your meds. Check your brain.
They’re watching.
Maeve Marley
November 9, 2025 AT 08:17I was skeptical about CBT-I-thought it was just ‘sleep hygiene’ fluff.
Then I did it.
Four weeks in, I stopped needing melatonin.
Eight weeks in, I stopped thinking about sleep.
That’s the magic: it stops being a battle.
Instead of fighting insomnia, you stop fighting yourself.
You learn to trust your body again.
It’s not about pills.
It’s about letting go.
And honestly? The best part isn’t sleeping better.
It’s waking up without guilt.
Like, ‘I didn’t need a chemical crutch today.’
That’s freedom.
ryan smart
November 10, 2025 AT 01:35Just take the pill. Stop overthinking.
It works. You feel better. End of story.
Why make it complicated?