Renal Dosing Calculator for Elderly Patients
Kidney Function Calculator
Use the Cockcroft-Gault formula to estimate creatinine clearance (CrCl) for patients over 65. This is critical for safe medication dosing.
Kidney Function Results
When kidneys slow down with age, even common medications can turn dangerous. About 38% of adults over 65 have chronic kidney disease, and many don’t even know it. That’s why a simple prescription for gabapentin, cefepime, or metformin can lead to falls, confusion, hospital stays, or worse - not because the drug is bad, but because the dose wasn’t adjusted for failing kidneys.
Why Kidney Function Matters More After 65
Your kidneys don’t just filter waste. They clear most drugs from your body. As you age, kidney function naturally declines. Glomerular filtration rate (GFR) drops by about 1% per year after age 40. By 70, many people have half the kidney function they had at 30. That means drugs that used to be cleared in 8 hours now stick around for 16, 24, or longer. The result? Toxic buildup.It’s not just about feeling sick. Too much digoxin can cause deadly heart rhythms. Too much lithium can lead to seizures. Too much metformin can trigger lactic acidosis. And these aren’t rare mistakes - 12-15% of all adverse drug events in older adults come from unadjusted kidney dosing.
How to Measure Kidney Function - and Why It’s Harder Than You Think
Doctors often rely on serum creatinine to estimate kidney function. But creatinine is misleading in older people. Muscle mass drops with age, so creatinine levels stay low even when kidneys are failing. That means standard tests can make your kidneys look better than they are.There are two main equations doctors use:
- Cockcroft-Gault (CG): Uses age, weight, sex, and serum creatinine. It’s older but more conservative - and that’s why it’s still preferred for dosing in the elderly.
- MDRD or eGFR: Estimates glomerular filtration rate. More accurate for younger people, but often overestimates kidney function in older adults by 15-20%.
Here’s the problem: if you use eGFR and it says your GFR is 31 mL/min, you might think you’re fine. But if Cockcroft-Gault says it’s 25, you’re actually in the danger zone for many drugs. That’s why KDIGO guidelines recommend using Cockcroft-Gault for dosing decisions in patients over 65 - even if eGFR looks okay.
For the most accurate picture, some clinics now use cystatin C, a newer marker that isn’t affected by muscle mass. But it’s not yet standard everywhere. If your doctor only checks creatinine, ask: “What’s my Cockcroft-Gault clearance?”
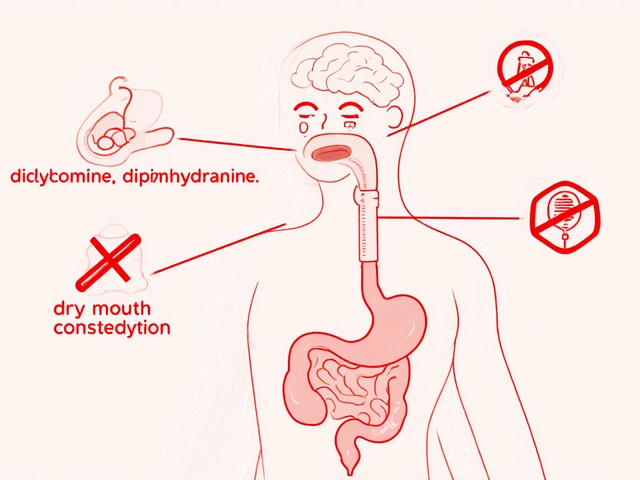
Which Medications Are Most Dangerous?
Not all drugs are created equal. Some are safe even with poor kidneys. Others need major changes - or should be avoided entirely.High-risk drugs (need strict adjustment):
- Digoxin: Therapeutic range is tiny - 0.8 to 2.0 ng/mL. Too much causes irregular heartbeat. Dose should be cut in half if CrCl is below 50 mL/min.
- Lithium: Used for bipolar disorder. Normal level is 0.6-0.8 mmol/L. If kidneys are impaired, levels can spike quickly. Check levels every 1-2 weeks after any dose change.
- Metformin: The go-to diabetes drug. But if CrCl is below 30 mL/min, it’s contraindicated. Even at 30-45 mL/min, use only the lowest dose and monitor closely. Many U.S. doctors still avoid it entirely in elderly patients.
- Gabapentin: Used for nerve pain. 90% is cleared by kidneys. Dose should drop from 300-1200 mg daily to 100-300 mg daily if CrCl is below 30 mL/min. 68% of prescribers get this wrong.
- Allopurinol: For gout. Standard dose is 100 mg/day. If CrCl is below 10 mL/min, start with 100 mg every other day. Too much can cause fatal skin reactions.
Drugs that are usually safe:
- Glipizide: Another diabetes drug. No dose adjustment needed, even with severe kidney disease.
- Cefdinir: Antibiotic. Just reduce frequency from twice daily to once daily if CrCl is below 30 mL/min.
- Vancomycin: Needs interval extension - not just dose reduction. Instead of every 12 hours, give every 48 hours in severe impairment.
Don’t assume a drug is safe just because it’s common. Always check the specific renal dosing rules.
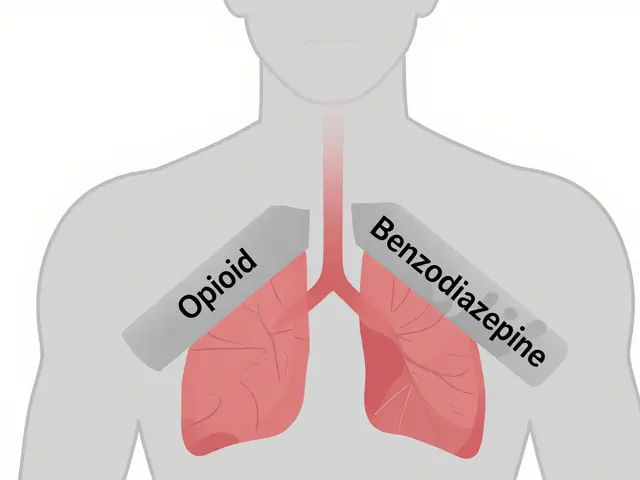
Three Ways to Adjust Dosing - and When to Use Each
There are three main strategies for adjusting meds when kidneys fail:- Dose reduction: Lower the amount per dose. Use this for drugs with narrow safety margins - like digoxin or lithium.
- Interval extension: Keep the same dose but give it less often. Works well for antibiotics like vancomycin or cefepime.
- Combination approach: Reduce dose AND extend interval. Used for drugs like piperacillin/tazobactam.
The “50% rule” - cut the dose in half if CrCl is below 50 mL/min - sounds simple. But it’s wrong for 22% of high-risk drugs. Vancomycin, for example, doesn’t respond well to dose cuts alone - you must extend the time between doses. That’s why blanket rules fail.
What Clinicians Get Wrong - And How to Fix It
A 2015 study found only 43.7% of doctors consistently adjusted doses for elderly patients. The biggest mistakes?- Using eGFR instead of Cockcroft-Gault for dosing
- Not checking drug metabolites - some drugs are safe, but their byproducts are toxic
- Assuming “no adjustment needed” means “no risk”
- Forgetting that over-the-counter drugs like NSAIDs (ibuprofen, naproxen) can worsen kidney function
One fix? Pharmacist-led reviews. At Mayo Clinic, when clinical pharmacists managed dosing for patients over 65, adverse drug events dropped by 58%.
Another? Electronic alerts. At the University of Nebraska Medical Center, an EHR alert system cut dosing errors by 37% in just one year.
Even simple tools help. Apps like Epocrates Renal Dosing are used over a million times a year. They give instant, evidence-based recommendations based on CrCl and drug.
What’s Changing in 2026 - And What to Watch For
The field is evolving fast. In 2023, the FDA approved the first AI-powered dosing tool, DoseOptima, which integrates with EHRs and predicts safe doses with 92.4% accuracy. It’s now being rolled out in major hospitals.KDIGO’s updated guidelines, expected in late 2023, now recommend cystatin C as the preferred test for elderly patients - because it’s not fooled by low muscle mass. More clinics are starting to use it.
Also watch for new pharmacogenomic research. The NIH is studying how genes affect how older adults clear drugs. In the future, your DNA might help determine your kidney-safe dose.
But the biggest barrier isn’t technology - it’s access. Only 63% of rural clinics have routine GFR testing. If you’re in a small town or long-term care facility, don’t wait for the system to catch up. Ask for your CrCl. Bring a list of all your meds. Say: “I’m over 65. Do any of these need adjusting for my kidneys?”
What You Can Do Today
You don’t need to be a doctor to protect yourself or a loved one. Here’s your action plan:- Know your CrCl. Ask your doctor for the Cockcroft-Gault calculation - not just eGFR.
- Review all meds twice a year. Include OTCs, supplements, and herbals. NSAIDs are especially risky.
- Use a pill organizer with reminders. Missed doses or doubled doses can both be dangerous.
- Carry a medication list. In an emergency, this could save your life.
- Speak up. If you feel dizzy, confused, or weak after a new prescription, say so. It could be toxicity.
Renal impairment isn’t a death sentence. With the right dosing, people with kidney disease live full, active lives. But getting it wrong? That’s preventable harm. The tools exist. The guidelines are clear. What’s missing is awareness - and the courage to ask the right questions.
How do I know if my kidney function is low?
Your doctor can estimate your kidney function using a blood test for creatinine and a formula like Cockcroft-Gault. The result is called creatinine clearance (CrCl). If your CrCl is below 60 mL/min, your kidneys are impaired. But don’t rely on eGFR alone - in older adults, Cockcroft-Gault is more accurate for dosing decisions. Ask for the specific number, not just “normal” or “abnormal.”
Can I still take metformin if I have kidney disease?
It depends. If your CrCl is below 30 mL/min, metformin should not be used. Between 30-45 mL/min, use only the lowest dose (500 mg once daily) and monitor kidney function monthly. Above 45 mL/min, it’s usually safe. Many doctors avoid metformin in elderly patients out of caution, but with careful monitoring, it’s one of the safest diabetes drugs available - if your kidneys can handle it.
Why is gabapentin so dangerous for older adults?
Gabapentin is cleared almost entirely by the kidneys. In elderly patients with reduced kidney function, it builds up and causes dizziness, confusion, and falls - which can lead to fractures or hospitalization. The most common error is giving the full adult dose. For CrCl under 30 mL/min, the dose should be reduced to 100-300 mg total per day - not 300 mg three times a day. Always check the dose based on CrCl, not age.
Should I stop all my medications if my kidneys are weak?
No. Stopping meds can be just as dangerous as taking too much. Many drugs can be safely used with proper dose adjustments. For example, glipizide works fine with poor kidneys, and some antibiotics just need less frequent dosing. The goal isn’t to stop everything - it’s to tailor each drug to your kidney function. Work with your doctor or pharmacist to find the right balance.
Can over-the-counter painkillers hurt my kidneys?
Yes. NSAIDs like ibuprofen, naproxen, and even aspirin (in high doses) reduce blood flow to the kidneys and can cause sudden kidney injury - especially in older adults. Acetaminophen (Tylenol) is safer for kidneys, but still needs caution if you have liver disease. Never take NSAIDs daily without checking with your doctor if you’re over 65 or have known kidney issues.
What should I bring to my doctor’s appointment about kidney dosing?
Bring a complete list of everything you take - including prescriptions, over-the-counter drugs, vitamins, supplements, and herbal remedies. Note any recent side effects like dizziness, confusion, nausea, or swelling. Ask: “Which of these drugs are cleared by my kidneys? What’s my CrCl? Do any need adjusting?” If you don’t know your CrCl, ask for it. Write it down.
Next Steps: What to Do If You’re at Risk
If you’re over 65 and take multiple medications, here’s your next move:- Call your doctor or pharmacist and ask for your latest Cockcroft-Gault CrCl result.
- Request a full medication review focused on renal dosing.
- Download a trusted app like Epocrates or Micromedex to check dosing guidelines yourself.
- Set a reminder to review your meds every 6 months - even if you feel fine.
- If you’re in a nursing home or long-term care facility, ask if they have a pharmacist on staff who reviews renal dosing.
Medication safety isn’t about complexity - it’s about attention. A simple question, a quick check, a small dose change - these can prevent a hospital stay, a fall, or worse. Your kidneys may be slowing down. But with the right knowledge, your meds don’t have to.



Andy Thompson
January 20, 2026 AT 21:41sagar sanadi
January 21, 2026 AT 06:17Art Gar
January 21, 2026 AT 20:58Edith Brederode
January 22, 2026 AT 09:21Renee Stringer
January 23, 2026 AT 08:12pragya mishra
January 24, 2026 AT 19:39kumar kc
January 24, 2026 AT 21:09Thomas Varner
January 24, 2026 AT 21:26clifford hoang
January 25, 2026 AT 05:19Arlene Mathison
January 26, 2026 AT 11:21Crystal August
January 28, 2026 AT 11:14Shane McGriff
January 29, 2026 AT 17:32