Many people take antispasmodics like dicyclomine or hyoscine for stomach cramps, irritable bowel syndrome, or bladder spasms. But what happens when you're also taking an antihistamine for allergies, an antidepressant for mood, or a sleep aid at night? These medications don’t just work in isolation-they can team up in dangerous ways. The real risk isn’t the antispasmodic itself, but what happens when it meets other drugs with similar effects. This isn’t theory. It’s happening in clinics, pharmacies, and homes every day.
How Anticholinergic Antispasmodics Work
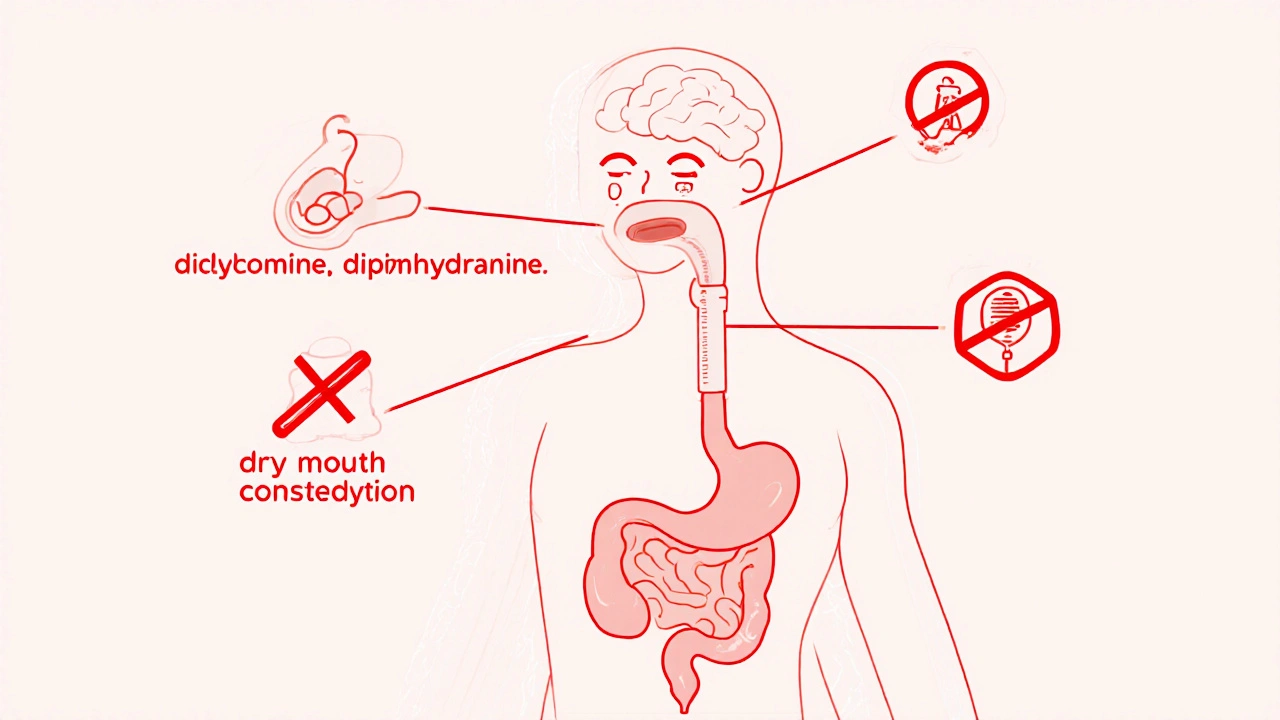
Antispasmodics like dicyclomine and hyoscine belong to a group called anticholinergics. They block a chemical in your body called acetylcholine. This chemical tells your muscles to contract-whether it’s your gut, bladder, or even your salivary glands. By blocking it, these drugs relax overactive muscles and ease cramps. But here’s the catch: acetylcholine isn’t just in your intestines. It’s everywhere. Your brain uses it for memory and focus. Your eyes use it to adjust focus. Your heart uses it to keep rhythm. When you block it in one place, you’re affecting multiple systems at once.
That’s why side effects like dry mouth, blurry vision, constipation, and trouble urinating are so common. In fact, a Mayo Clinic study found that 69% of people taking high doses of dicyclomine experienced side effects-compared to just 16% on a placebo. These aren’t rare glitches. They’re predictable outcomes of how the drug works.
The Hidden Problem: Additive Effects
The biggest danger isn’t one anticholinergic drug. It’s multiple ones taken together. Think of it like stacking weights. One anticholinergic might cause mild dry mouth. Add another-say, diphenhydramine (Benadryl)-and now you’re dealing with confusion, dizziness, or even hallucinations. This isn’t speculation. It’s documented in the American Geriatrics Society Beers Criteria®, which lists several antispasmodics as potentially inappropriate for older adults because of their high anticholinergic burden.
Many common medications you wouldn’t think of as anticholinergics actually are. Antidepressants like amitriptyline and nortriptyline. Antipsychotics like quetiapine. Even some allergy pills and motion sickness patches. A patient taking dicyclomine for IBS might also be on amitriptyline for nerve pain. On paper, both are fine. Together? They can turn mild constipation into a medical emergency. One patient on Drugs.com reported: “When I started amitriptyline, my dicyclomine stopped working-and I couldn’t go to the bathroom for five days.” That’s not an isolated story. Pharmacists on Reddit say they’ve had to step in multiple times a month when patients get prescribed overlapping anticholinergics by different doctors.
Who’s at Highest Risk?
Older adults are the most vulnerable. As we age, our bodies process drugs differently. Liver and kidney function slow down. The blood-brain barrier becomes leakier. That means anticholinergics enter the brain more easily and stick around longer. A 2023 study in JAMA Internal Medicine showed that people over 65 on multiple anticholinergic drugs had a 50% higher risk of delirium-a sudden, dangerous state of confusion that can lead to falls, hospitalization, or even death.
But it’s not just age. People with glaucoma, enlarged prostate, or certain heart conditions are also at higher risk. The FDA has boxed warnings for anticholinergics in these groups. And if you’re on a monoamine oxidase inhibitor (MAOI) for depression, mixing it with hyoscine can trigger life-threatening high blood pressure.

Common Dangerous Combinations
Here are real-world examples of combinations that can cause trouble:
- Dicyclomine + Amitriptyline: Both block acetylcholine. Together, they can cause severe constipation, urinary retention, and cognitive fog.
- Hyoscine + Diphenhydramine (Benadryl): This combo is a classic trap. One for motion sickness, one for allergies. Both cause drowsiness and confusion. Elderly patients often end up in the ER after this mix.
- Oxybutynin + Tolterodine: Both treat overactive bladder. Prescribing both is common-but doubling up on anticholinergics multiplies side effects without improving results.
- Antispasmodic + Alcohol or Benzodiazepines: Alcohol and sleep aids like lorazepam also depress the central nervous system. Add anticholinergics, and you’re looking at extreme drowsiness, slowed breathing, or even coma.
These aren’t rare cases. A 2022 IMS Health report found that nearly 40% of patients on anticholinergic antispasmodics were also taking at least one other anticholinergic medication-often without their doctor knowing.
How to Spot the Risk
There’s a tool doctors now use called the Anticholinergic Cognitive Burden Scale. It ranks over 100 common medications on a scale from 0 (no anticholinergic effect) to 3 (strong effect). If your total score is 2 or higher, you’re at increased risk for side effects. Many hospitals now use electronic systems that flag these combinations automatically.
But you don’t need a system to protect yourself. Ask yourself:
- Are you taking more than one medication for stomach, bladder, or sleep issues?
- Do you feel unusually dry-mouthed, constipated, or confused after starting a new drug?
- Have you been prescribed medications by more than one doctor without a full medication review?
If you answered yes to any of these, you need to talk to your pharmacist or doctor. Don’t wait for symptoms to get worse.

What Are the Alternatives?
The good news? You don’t have to stick with anticholinergics. Many newer options exist with far fewer interactions.
For irritable bowel syndrome, drugs like eluxadoline or rifaximin work without blocking acetylcholine. For bladder spasms, mirabegron targets a different receptor entirely and has a much cleaner safety profile. Even non-drug options like pelvic floor therapy, dietary changes, or stress management techniques can reduce symptoms without any drug risk.
In fact, the American Gastroenterological Association now recommends non-anticholinergic treatments as first-line for most functional GI disorders. Why? Because the risks of anticholinergics now outweigh the benefits for most people-especially when safer choices exist.
What to Do Next
If you’re on an antispasmodic:
- Make a full list of every medication you take-prescription, over-the-counter, supplements, and herbal products.
- Check each one against the Anticholinergic Burden Scale (available online from the University of Washington).
- Bring the list to your doctor or pharmacist. Ask: “Could any of these be interacting with my antispasmodic?”
- Don’t stop any medication on your own. But do ask if there’s a safer alternative.
Many people assume that because a drug is prescribed, it’s safe to combine. That’s not true. The truth is, anticholinergic antispasmodics are becoming less common-not because they don’t work, but because we now know how risky they can be when layered with other meds.
There’s no shame in asking for a better option. Your body isn’t designed to handle multiple drugs that silence the same chemical signal. The goal isn’t just to treat a cramp-it’s to do it without risking your brain, your bladder, or your safety.
Can I take antispasmodics with over-the-counter sleep aids?
No, it’s risky. Many OTC sleep aids like Unisom or Nytol contain diphenhydramine or doxylamine-both strong anticholinergics. Combining them with dicyclomine or hyoscine can cause severe drowsiness, confusion, trouble urinating, or even delirium, especially in older adults. Always check the active ingredients before combining any sleep aid with an antispasmodic.
Are there antispasmodics without anticholinergic effects?
Yes. For bladder spasms, mirabegron works by relaxing the bladder muscle through a different mechanism and has minimal anticholinergic side effects. For IBS, rifaximin and eluxadoline are non-anticholinergic options. Even peppermint oil capsules have shown effectiveness for cramping without affecting acetylcholine. Ask your doctor if one of these alternatives is right for you.
Why do some doctors still prescribe anticholinergic antispasmodics?
They’re cheap, widely available, and have been used for decades. Many doctors learned to prescribe them in medical school and haven’t updated their practice. But guidelines have changed. The American Gastroenterological Association now recommends avoiding them as first-line treatment. If your doctor prescribes one without discussing risks or alternatives, it’s okay to ask: “Is there a safer option?”
Can anticholinergic interactions cause long-term damage?
Yes. Studies link long-term use of multiple anticholinergic drugs to an increased risk of dementia, especially in people over 65. A 2023 study in The Lancet found that people who took high anticholinergic burden medications for three years or more had a 54% higher risk of developing dementia. This doesn’t mean every short-term use causes damage-but chronic, combined use is a known risk factor.
How can I check if my meds have anticholinergic effects?
Use the Anticholinergic Burden Calculator from the University of Washington. It’s free, online, and lets you search by drug name. You can also ask your pharmacist to run your list through their system. Many pharmacies now have tools that flag high-risk combinations automatically. Don’t guess-get it checked.
Final Thoughts
Antispasmodics aren’t inherently bad. But their anticholinergic nature makes them a ticking time bomb when mixed with other common meds. The shift away from these drugs isn’t about new science-it’s about common sense. We now know that blocking acetylcholine in one part of the body can quietly break things in others. The best treatment isn’t always the one that’s been around the longest. It’s the one that works without putting your brain, bladder, or balance at risk.






Brad Seymour
November 8, 2025 AT 07:45Man, I had no idea my nightly Benadryl was basically a chemical handshake with my dicyclomine. My grandma used to say ‘don’t mix meds like cocktails’ - turns out she was a genius. Just cut the diphenhydramine and switched to melatonin. No more brain fog at 3 a.m.
Alyssa Salazar
November 8, 2025 AT 11:53Let’s be real - anticholinergic burden is a legit pharmacokinetic nightmare. The ACCS scale isn’t just a gimmick; it’s clinical gospel. If your total score hits ≥2, you’re playing Russian roulette with your hippocampus. Seriously, stop self-medicating with OTC sleep aids and start using PharmGKB or Lexicomp. Your neurocognitive reserve will thank you.
Malia Blom
November 10, 2025 AT 07:20Oh wow, another ‘big pharma is evil’ post. Let me guess - you’re also mad that aspirin causes stomach bleeds and Tylenol kills livers? Everything’s toxic if you stack it wrong. Maybe the real problem is people who think they know pharmacology after reading one article on Reddit. My 78-year-old aunt takes 8 meds including dicyclomine and amitriptyline - she’s sharper than my therapist. Stop fearmongering.
Erika Puhan
November 12, 2025 AT 03:57Typical American medical ignorance. In India, we don’t just throw anticholinergics at every cramp. We use Ayurvedic herbs like ajwain and ginger - no CNS depression, no dementia risk. You guys treat symptoms like puzzles to be solved with more pills. Pathetic. Your healthcare system is a corporate dumpster fire.
Edward Weaver
November 13, 2025 AT 09:01So you’re telling me I can’t take my Unisom with my IBS med? That’s why America’s going to hell. We used to be able to sleep and not feel like a zombie. Now we gotta consult a pharmacist like we’re launching a rocket. I’m not some geriatric lab rat. I’m a veteran. I’ve earned the right to sleep.
Lexi Brinkley
November 14, 2025 AT 22:55OMG YES. I was on dicyclomine + Benadryl for months and thought I was just ‘getting old’. Then my pharmacist said ‘you’re basically sedated by two brain-slowing drugs’ 😱 I switched to mirabegron and now I’m actually awake during Zoom calls again. 🙌
Kelsey Veg
November 16, 2025 AT 11:18so like… i took dicyclomine and then took a nyquil cause i had a cold and then i couldnt pee for 2 days?? and my head felt like mush?? is that normal?? or am i just dumb??
Alex Harrison
November 18, 2025 AT 09:09Just wanted to say I read this whole thing and it made me check my meds. Turned out I was on oxybutynin and amitriptyline. My doc never told me they were both anticholinergic. I’ve been constipated for months and thought it was just my diet. Changed meds last week - already feel better. Thanks for the wake-up call.
Jay Wallace
November 19, 2025 AT 14:40...and yet, the FDA still approves these combinations. How many people have to end up in the ER before the system stops being a revolving door of polypharmacy? The real scandal isn’t the drugs - it’s that doctors don’t even bother checking for interactions anymore. It’s all about the billing code, not the patient. Wake up, America. We’re being medicated into oblivion.
Cris Ceceris
November 20, 2025 AT 13:23It’s wild how we treat the body like a machine with separate compartments. Block acetylcholine in the gut? Fine. But it’s not a switch - it’s a network. That same chemical helps you remember your kid’s birthday, focus at work, and not pee your pants. We’re not just treating cramps - we’re tuning a symphony with a hammer. And now we’re learning that some of the instruments are made of glass.
I’ve been on mirabegron for six months now. No dry mouth. No brain fog. Just relief. It’s like switching from a steam engine to an electric car - same destination, way less noise.
And honestly? The fact that we’re still prescribing dicyclomine like it’s 1985 says more about medical inertia than medical science. We know better. We just don’t always do better.
Alyssa Fisher
November 21, 2025 AT 13:49There’s a quiet epidemic here - and it’s not just the drugs. It’s the assumption that if a doctor writes it, it’s safe. But doctors are human. They’re rushed. They specialize. One prescribes for IBS, another for depression, another for sleep. No one sees the whole picture. That’s why pharmacists are the unsung heroes of medication safety. If you’re on more than three prescriptions, schedule a med review. Not next month. Now.
And yes - peppermint oil capsules work. Double-blind studies show they’re as effective as antispasmodics for IBS with zero anticholinergic load. It’s not ‘alternative medicine.’ It’s evidence-based, low-risk, and available at any grocery store.
Rashmi Mohapatra
November 23, 2025 AT 13:40lol u think ur smart for switching to mirabegron? in my village we just drink warm water with lemon and sit on a hot stone. no pills. no science. just wisdom. u guys are too lazy to feel your own body. u just want a pill for everything.
Abigail Chrisma
November 23, 2025 AT 13:47As a nurse who’s worked in geriatrics for 20 years, I’ve seen this play out too many times. A patient comes in confused, constipated, barely able to walk - and it’s because they’re on three anticholinergics and a benzodiazepine. We call it ‘anticholinergic syndrome.’ It’s reversible. But only if someone catches it in time.
My advice? Make a medication list. Write it down. Bring it to every appointment. Even if your doctor says ‘I know what you’re on,’ show them anyway. You’re the only one who knows your full story.
And if you’re older? Please, please don’t take Benadryl for sleep. There are safer options. Your brain matters more than a few extra hours of unconsciousness.
Andy Slack
November 25, 2025 AT 10:04Just got off the phone with my pharmacist. She flagged my combo: dicyclomine + nortriptyline + diphenhydramine. Total burden: 7. I nearly passed out. She set me up with a telehealth consult for mirabegron and cognitive behavioral therapy for my IBS. I’m not just surviving anymore - I’m living. This post saved me. Thank you.