If you grabbed a random medicine cabinet and poked through the shelves, you’d probably run into erythromycin somewhere. It’s been called the backup, the lifesaver, sometimes the hero when penicillin just isn’t an option. This medicine’s been tossed around by doctors since the 1950s, and it’s still going strong—fighting bacterial infections from stubborn pimples to serious cases of pneumonia. But behind that well-worn name, there’s plenty folks don’t realize. Think you know how antibiotics work? Erythromycin’s story is full of two-edged swords, surprising perks, and a bunch of modern twists that nobody really tells you about at the doctor’s office.
How Erythromycin Works and What It’s Really For
You’ve probably heard a million times: finish your antibiotics, or risk making bacteria stronger. But with erythromycin, there’s more in play than the usual warnings. It belongs to a group called macrolide antibiotics. What that means in plain talk? When it gets in your system, erythromycin stops bacteria from making the proteins they need to grow and multiply. In the right dose, it basically puts the germs on ice so your body’s natural defenses can mop them up.
Doctors pull out erythromycin when a patient can’t hack penicillin (think bad allergies or certain resistant bugs). It’s not just a backup, though. The stuff is especially good against illnesses like whooping cough (pertussis), certain kinds of pneumonia (caused by Mycoplasma or Legionella), skin infections, and even some eye stuff (like conjunctivitis in newborn babies). If your acne seems to laugh at drugstore creams, there’s a good chance a dermatologist will pop up with an erythromycin prescription. Beyond that, it’s also used to help people heading for surgery—keeping possible infections at bay when they’re at their most vulnerable.
One thing a lot of folks miss: erythromycin isn’t magic. It doesn’t touch viruses (sorry, it’s no use against colds or the flu). Doctors sometimes hear demands for antibiotics to wipe out viral woes, but dishing it out that way just breeds resistance. Real talk? Use erythromycin only when a real, proven bacterial villain is at work. Here’s a quick data bite: according to the CDC’s 2024 report, unnecessary antibiotic use dropped by 17% in clinics that added a quick test for strep throat or pertussis. It saves a lot of trouble, not just for you, but for everyone who might need antibiotics down the road.
If you’re looking at the ingredient list, you might spot names like EES, Ery-tab, and even topical gels—all with erythromycin at the core. It even comes as an eye ointment (doctors like this for treating newborn babies, protecting their vision from sneaky hospital bacteria). The form you get will totally depend on the kind of infection you’re fighting and what your doctor thinks is the best route.
Before you grab a bottle: don’t forget to tell your doc about anything weird in your bloodwork, your liver health, or if you pop antacids regularly. Erythromycin likes to play games with drug metabolism, so a single detail can make a world of difference in how it works for you.
Erythromycin: Surprising Facts, Smart Tips, and Need-to-Know Warnings
Have you ever finished a round of antibiotics only to have an upset stomach for days? Erythromycin is infamous for this. In fact, if you ask two people who’ve taken it, at least one might mention they were glued to the bathroom for a while. About 10–15% of patients say nausea or diarrhea shows up. That’s because erythromycin amps up gut motility—sometimes doctors even use it (on purpose!) for folks whose stomachs aren’t working quickly enough. Bit ironic, isn’t it?
So how do you dodge the worst side effects? Here are some hard-learned tips:
- Take it with food if your stomach is sensitive—though some formulas work best on an empty stomach, your doctor or pharmacist will give you the right instructions for what you’re prescribed.
- Drink lots of water. Dehydration and antibiotics do not play nice together.
- Watch out for antacids! They can mess with how your body absorbs erythromycin, especially the old-school formulations.
- If the diarrhea’s really bad or you spot blood or mucus, call your doctor right away. Rarely, antibiotics can trigger a nasty gut infection called C. difficile.
- If you get a rash, hives, or trouble breathing, don’t mess around—go to urgent care. Allergic reactions to erythromycin aren't super common, but they can get real serious, real fast.
Thinking about mixing meds? Erythromycin goes nuclear with certain drugs. There’s a reason doctors double-check any cholesterol-lowering pill (statins) you’re on—some combos can cause dangerous muscle damage. Blood thinners, heart meds (especially digoxin), anticonvulsants, even some antihistamines—this isn’t just doctor drama, it’s proven stuff. As an example, a 2023 study in the journal "Clinical Pharmacology" found rates of heart rhythm trouble nearly doubled for folks mixing erythromycin with a type of antihistamine called loratadine. That’s not something you want turning up in your week.
Here’s a quick table showing common meds that can make taking erythromycin a risk:
| Drug Type | Example | Possible Effect with Erythromycin |
|---|---|---|
| Statins (cholesterol) | Simvastatin, lovastatin | Muscle damage (rhabdomyolysis) |
| Heart rhythm meds | Amiodarone, sotalol | Heart arrhythmia |
| Blood thinners | Warfarin | Increased bleeding risk |
| Anticonvulsants | Carbamazepine | Toxicity/headache/confusion |
| Antihistamines | Loratadine, terfenadine | Dangerous heart rhythms |
Ever hear about erythromycin causing sun sensitivity? That’s one you won’t find in every patient leaflet, but a handful of real cases say it can happen, especially if you’re already prone to sunburns. If you’re going to be outside for a while, toss on some SPF just in case. Don’t trust cloudy days either—UV sneaks through faster than you think.
Now, about the little ones—erythromycin stays popular for newborns to keep them safe from a type of conjunctivitis picked up during birth. For babies, doctors use lower doses and lean on ointment for the eyes, because their little livers can’t handle the full tablet blast. As for older kids and teens, if they’re allergic to penicillin or have a chest infection, erythromycin’s a solid plan B.
Pregnant or breastfeeding? Good news—erythromycin is usually considered safe, but only if there’s a genuine infection that needs tackling. Your doctor will weigh risk versus benefit, especially in early pregnancy. There’s some debate (and a few mixed studies) about certain forms causing mild liver effects, but these are rare and usually cleared up with careful monitoring.
One oddball fact: erythromycin isn’t just an antibiotic. Scientists use low doses in the lab to make cells grow better, and some hospitals use its stomach-speeding superpower for patients who need tubes placed in their guts. Wild, right?

Modern Use in 2025: Erythromycin’s Role, Resistance Patterns, and Future Tips
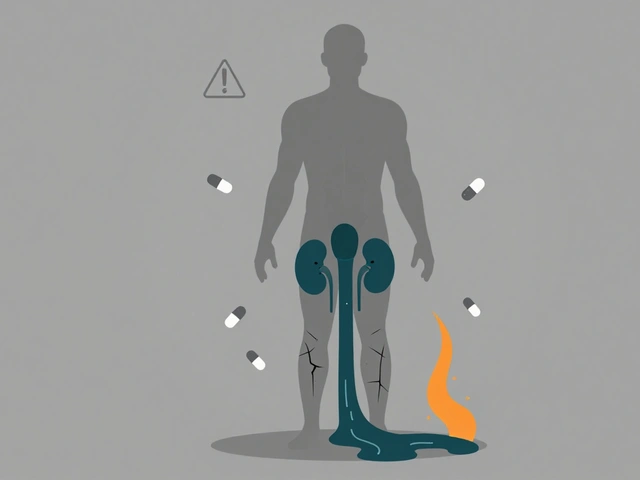
So why is erythromycin still sitting on pharmacy shelves when flashier antibiotics come out every year? Easy answer: resistance. Bacteria aren’t stupid—they learn quick. Doctors have to keep a lineup of go-to meds that attack illness in different ways, and erythromycin still fills unique roles. The latest CDC stats (spring 2025) show resistance rates for erythromycin hover around 22% in some common Streptococcus species—higher than we’d like, but lower than the worst-case with older tetracycline drugs.
This matters for anyone with chronic conditions (think COPD or recurrent bronchitis), where repeat infections need careful planning. Your doctor may run a culture and sensitivity test before handing over an erythromycin script. That way, you know the pill will actually work.
Here are some tips to get the most out of your prescription in this post-pandemic world:
- Don’t self-diagnose. With resistance on the rise and new variants floating around in 2025, don’t pull out leftover antibiotics without an actual test showing a bacterial infection.
- Store erythromycin properly. Room temp, away from light for pills, and in the fridge if you have a liquid form—kids’ suspensions especially go bad quickly if left out.
- Never split or crush extended-release tablets. They’re designed to drip medicine over several hours. Break that barrier, and you could zing your system with too much at once.
- If your symptoms aren’t clearing up in a couple of days, call your doctor. You might have a bug that laughs at erythromycin or even a virus instead.
- Return any leftover antibiotics to a safe disposal site. Don’t save them ‘for next time’—outdated meds can lose punch and breed resistance if misused.
Modern medicine moves fast. Erythromycin’s an old drug, but it’s earned its spot. Newer options are swapped in when bacteria get too cocky, but it turns out, the classics still work—if you use them wisely. Just remember: the real enemy is the wrong use, not the medicine itself. With smart teamwork between you and your healthcare team, erythromycin stays a valuable tool to keep stubborn bacteria from turning into a bigger problem for everyone.





Dan Burbank
July 18, 2025 AT 13:14Honestly, erythromycin often gets more credit than it deserves in the antibiotic pantheon. Sure, it’s versatile and all that, but when you break down its pharmacological efficiency and side effect profile, you start to see the cracks. It’s not the silver bullet some make it out to be.
The fact that it has so many drug interactions and can cause gastrointestinal unrest at such a high rate is problematic, especially compared to newer macrolides with improved tolerability. And don’t even get me started on resistance patterns.
For anyone seriously invested in understanding antimicrobials, this guide might be a good refresher, but don’t be fooled into thinking erythromycin is a go-to without caveats. It’s not a one-size-fits-all solution, despite the marketing push.
Anna Marie
July 21, 2025 AT 20:34I appreciate the detailed overview here. From a patient care perspective, knowing the potential side effects and interactions can really help mitigate risks associated with erythromycin use. Sometimes, when we prescribe antibiotics, patients aren’t fully aware of what to look out for.
It's crucial that such information is accessible and clear, especially for those starting treatment who might be overwhelmed by medical jargon. This guide does a decent job explaining things in plain terms, which I find helpful.
Anyone else feels like patient education is still the weak link when it comes to antibiotic use?
Abdulraheem yahya
July 24, 2025 AT 19:01This is quite an informative post, thank you for sharing. In my experience working in diverse healthcare settings, erythromycin remains a staple, especially when other antibiotics aren’t an option due to allergies or resistance.
Though it’s true the side effects can be harsh, careful monitoring and patient counseling often tip the balance in favor of its use. Plus, don’t underestimate the ease of use in certain formulations which really helps with compliance in some communities.
Hopefully, future iterations of such guides keep integrating global perspectives since the antibiotic landscape is ever so dynamic, particularly with resistance trends evolving rapidly worldwide.
Preeti Sharma
July 28, 2025 AT 02:21Why do we continue to glorify antibiotics like erythromycin without simultaneously addressing the root cause of infections, i.e., the underlying environment and lifestyle factors? I find that this conversation often sidesteps deeper reflections about over-reliance on pharmaceuticals as a crutch.
It’s fascinating, really, how society elevates these molecules to savior status while rarely contemplating the philosophical implications of medical interventionism. We're so infatuated with treatment that prevention seems secondary.
That said, the guide offers practical info, but I wish it nudged readers to think beyond mere pharmacology towards holistic health.
Ted G
July 31, 2025 AT 09:41Watch out, folks. Erythromycin is one piece in a much bigger puzzle and a tool often exploited by pharmaceutical interests to keep us dependent on meds. I’m skeptical about any antibiotic with broad claims about safety and efficacy claiming it’s perfectly fine in 2025 when resistance is escalating.
Who benefits from all this? Certainly the big pharma giants pushing reformulated versions and new patents. This guide, while useful, should be read with a pinch of salt, always question the narrative.
Ask yourself: are we treating symptoms or are we being treated as mere consumers?
Miriam Bresticker
August 3, 2025 AT 17:01OMG this erythromycin guide is super comprehensive lol ✨ I love how it breaks down the side effects cuz sometimes u just want the facts straight up. Also would be cool if they included some emoji or something to spice up the reading experience 😂 but serious tho, it's good info.
Has anyone here had wild reactions to it? That tummy thing it mentions is no joke. Personally, I try to listen to my body and adjust if something feels off. Antibiotics like this are no joke, gotta respect them.
Claire Willett
August 7, 2025 AT 00:21This guide contains some vital clinical pearls for erythromycin administration. Notably, its influence on cytochrome P450 enzymes demands judicious consideration when polypharmacy is involved.
Moreover, clinicians must weigh erythromycin's therapeutic index carefully against potential QT prolongation risks, particularly in at-risk populations.
In short, while erythromycin remains relevant, its application warrants scrupulous attention to pharmacokinetic and dynamic parameters to mitigate adverse outcomes effectively.
Keli Richards
August 10, 2025 AT 07:41I actually found this guide to be pretty user-friendly, which is a relief when it comes to complicated stuff like antibiotics. I think the tips on interactions and side effects are especially helpful because sometimes the warnings you get from doctors or pharmacists fly over your head if you don’t have a medical background.
It would be even better if they added more info on what to do if you notice side effects starting to show up though. Like, quick steps or when to call your doctor or urgent care.
Still, in the big picture, this kind of resource is definitely useful for patients and caregivers trying to navigate treatment safely.
Ravikumar Padala
August 13, 2025 AT 15:01While I acknowledge the widespread use of erythromycin, I can't help but feel uninterested in prolonged discussions about its nuances. The guide seems adequate, but I've skimmed through and found no earth-shattering revelations. Antibiotics are what they are, and erythromycin is just one of them.
That said, it's useful enough for the curious but let's not pretend this is a masterpiece of medical literature.
King Shayne I
August 16, 2025 AT 22:21I gotta say, this whole guide is fluff unless it tackles the uncomfortable truths about antibiotic overuse and resistance. Erythromycin is pushed too much as a first resort by careless practitioners. It’s a real hazard when misused, and guides like this need to be more blunt about that reality.
People need to understand there’s a line between necessary use and reckless prescriptions that fuel superbugs. If not addressed, this kind of content just becomes corporate noise.
jennifer jackson
August 17, 2025 AT 13:14Really grateful for this article! It’s reassuring to have a go-to source that lays out the uses and side effects so clearly without freaking anyone out. I personally hate feeling left in the dark about what meds do inside my body.
I think tips like these empower patients to take control of their health journey rather than just blindly following prescriptions. Having knowledge makes you less vulnerable.
Stay optimistic everyone — antibiotics are powerful allies when used wisely 🌟