When your asthma isn’t responding to your inhaler, it’s not always because you’re not using it right. Sometimes, the problem is deeper-your airways are still inflamed, even if you feel okay on most days. That’s where FeNO testing comes in. It’s not a new idea, but it’s becoming a game-changer in how doctors understand and treat asthma today.
What FeNO Testing Actually Measures
FeNO stands for Fractional Exhaled Nitric Oxide. It’s a simple breath test that measures how much nitric oxide is in your exhaled air. Sounds strange? Nitric oxide isn’t just a pollutant-it’s a natural molecule your body makes when there’s inflammation in your airways. In asthma, especially the type driven by allergies or eosinophils (a kind of white blood cell), your body produces more of it. Higher levels mean more inflammation.
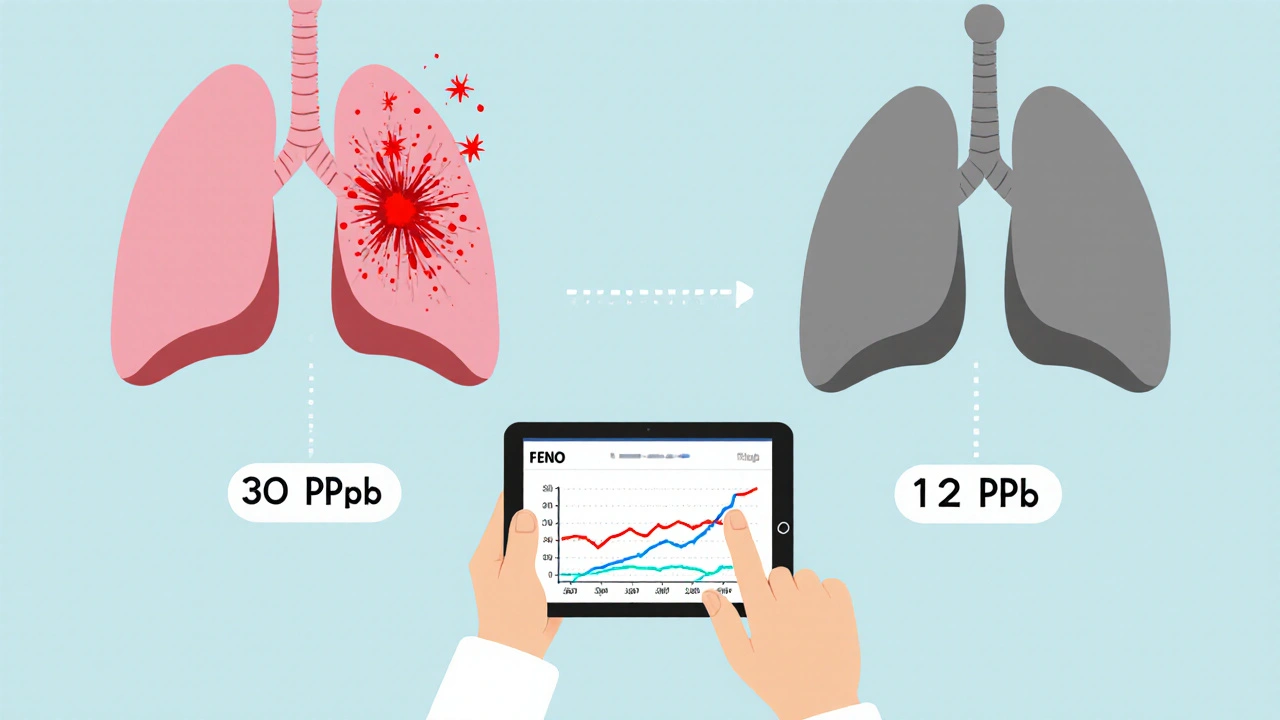
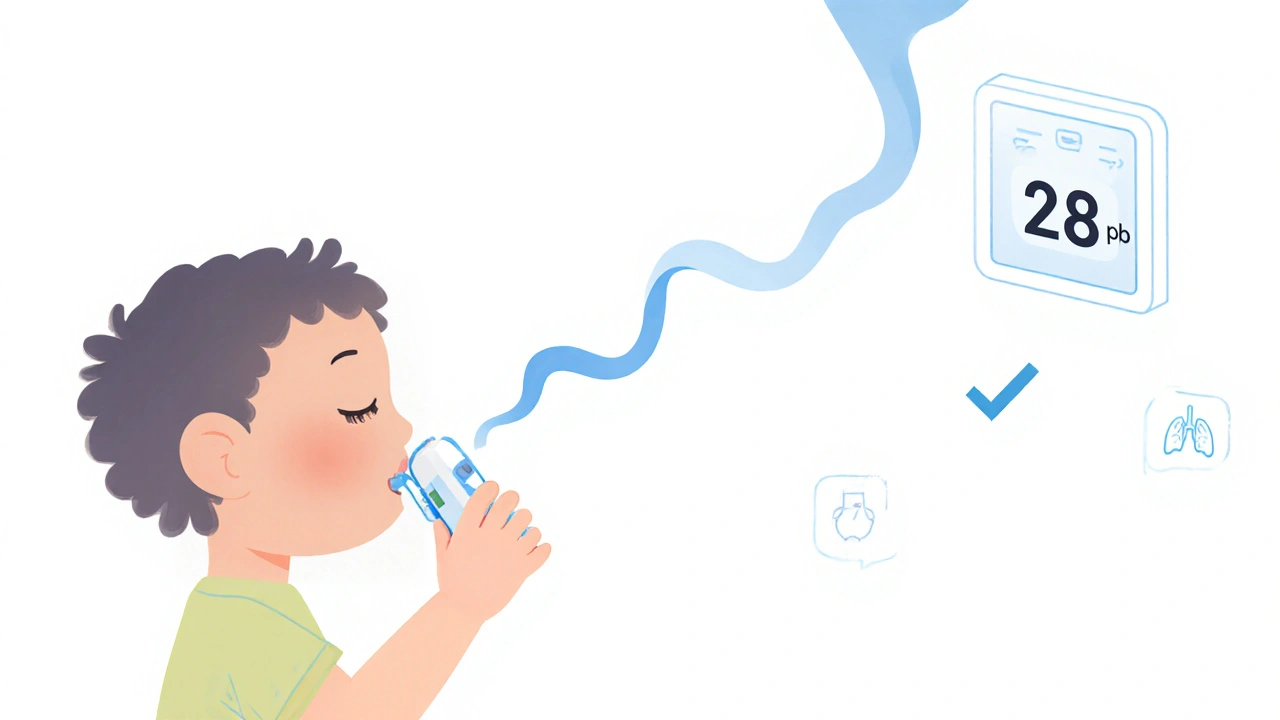
The test itself takes less than a minute. You breathe in through a filter that cleans out outside air, then slowly blow into a handheld device for about 10 seconds. No needles. No blood. No discomfort. Even kids as young as five can do it. The device gives a number in parts per billion (ppb). In adults, a reading of 25 ppb or higher suggests significant airway inflammation. For kids between five and twelve, it’s 20 ppb or higher.
It’s not magic-it’s science. This method grew out of Nobel Prize-winning research in the 1990s on how nitric oxide works in the body. By the early 2000s, doctors realized they could use it to see inside the lungs without poking or prodding.
Why FeNO Beats Traditional Tests in Some Cases
Most people with asthma get spirometry-a lung function test where you blow hard into a tube. But spirometry only tells you how well your lungs are moving air. It doesn’t tell you why they’re struggling. Two people can have the same spirometry results but very different levels of inflammation. One might need a steroid inhaler; the other might need something else entirely.
FeNO fills that gap. It’s not great at ruling asthma out (it misses some cases), but it’s excellent at confirming it when inflammation is present. Studies show that if your FeNO level is high, you’re up to seven times more likely to have asthma than someone with a normal reading. That’s powerful when you’ve been told you have “chronic bronchitis” for years but your symptoms don’t match.
Compared to blood tests for eosinophils or sputum analysis (which requires coughing up mucus), FeNO is faster, easier, and more comfortable. You get results while you’re still sitting in the chair. No lab delays. No waiting days for results.
How Doctors Use FeNO to Change Treatment
FeNO isn’t just for diagnosis. It’s used to manage asthma over time. If you’re on a daily steroid inhaler but still having flare-ups, your doctor might check your FeNO level. If it’s still high, your current dose isn’t controlling the inflammation. That’s when they might increase your medication or switch you to a biologic therapy-like dupilumab or benralizumab-which targets inflammation at the source.
Research shows that using FeNO to guide treatment can cut asthma flare-ups by nearly half. One study found patients who had their treatment adjusted based on FeNO levels had fewer ER visits and hospital stays. That’s not just better quality of life-it saves money. Asthma costs the U.S. over $56 billion a year, mostly from preventable emergencies.
Doctors typically test FeNO every 3 to 4 months if you’re on maintenance therapy. More often if you’re changing medications. The key is tracking trends-not just one number. A rising FeNO level over time is a red flag, even if you feel fine.
Limitations and When FeNO Doesn’t Help
FeNO isn’t perfect. It only picks up type 2 inflammation-the kind tied to allergies and eosinophils. If your asthma is triggered by cold air, exercise, or stress without this type of inflammation, your FeNO level might be normal. That doesn’t mean you don’t have asthma. It just means this test won’t catch it.
Smoking can drop FeNO levels by 30-50%, making results misleading. Recent steroid use-even a single dose-can also lower readings. That’s why you’re told not to smoke, eat, drink (except water), or exercise for an hour before the test.
And here’s the biggest catch: FeNO should never be used alone. The American Thoracic Society and NICE guidelines both say it’s an adjunct tool. You still need your symptoms, lung function tests, and medical history. A high FeNO level in someone with no wheezing or breathing trouble might just mean they have allergic rhinitis-not asthma. A low FeNO in someone with severe symptoms? That could mean non-eosinophilic asthma, which needs a different approach.
What Patients Say About FeNO Testing
Real people are noticing the difference. On patient forums, 87% of those who’ve had the test say it was easy. One person wrote: “I blew into a tube for 10 seconds. Got my result before my spirometry even finished. My doctor finally understood why my inhaler wasn’t working.”
Many say it helped them get off the “trial-and-error” cycle. “I was on three inhalers for two years,” shared a Reddit user. “FeNO showed my inflammation was still high. My doctor switched me to a biologic. I haven’t had a flare-up since.”
But not everyone has access. In the U.S., only 58% of commercial insurance plans cover FeNO without extra hurdles. Some patients report being denied coverage even after multiple flare-ups. Rural clinics are even less likely to have the equipment-only 22% offer it, compared to 67% in cities.
What’s New in FeNO Technology
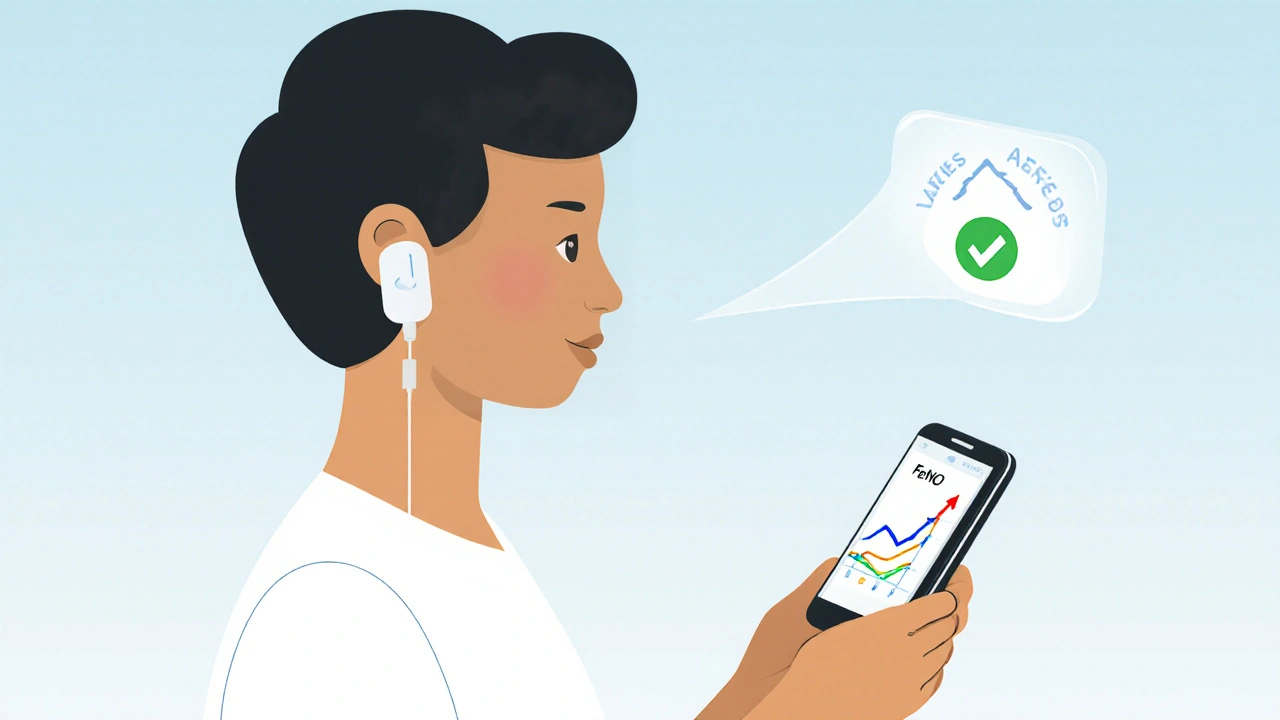
The field is evolving fast. In early 2023, the FDA cleared the first smartphone-connected FeNO device. It’s a small, portable unit you plug into your phone. You can test yourself at home and send results directly to your doctor. The price? Around $299. It’s not covered by insurance yet, but for people with frequent exacerbations, it might be worth it.
Devices like the NIOX VERO® and NObreath® now include real-time visual feedback-showing you if you’re blowing too fast or too slow. That cuts down on invalid tests from 20% to under 5%. Better technique means better data.
European guidelines now recommend FeNO to predict who will respond to expensive biologic drugs. That’s huge. These treatments cost over $30,000 a year. FeNO helps make sure they’re only given to people who will actually benefit.
How to Get the Most Out of FeNO Testing
If your doctor suggests FeNO testing, here’s how to make sure it’s useful:
- Follow prep rules: no smoking, eating, drinking (except water), or exercise for one hour before.
- Don’t do it right after using your rescue inhaler. Wait at least 4 hours.
- Ask to see your results and track them over time. Look for trends, not single numbers.
- Ask how it fits with your other tests-spirometry, symptom logs, peak flow readings.
- If your insurance denies coverage, ask for a letter of medical necessity from your doctor. Many appeals succeed when you show a pattern of uncontrolled asthma.
FeNO testing isn’t the end-all-be-all of asthma care. But when used right, it turns guesswork into clarity. It gives doctors a window into your lungs you can’t see with a stethoscope. And for patients stuck in cycles of ineffective treatment, it’s often the missing piece they’ve been waiting for.
What’s Next for FeNO?
Researchers are now studying whether FeNO can predict who will respond to new asthma drugs before they even start treatment. Large studies like the NIH’s PREPARE-Asthma trial are looking at FeNO across diverse populations-children, older adults, people of different ethnic backgrounds-to make sure the test works equally well for everyone.
Standardization is still a challenge. Different devices can give slightly different readings. But as more clinics adopt the test and digital platforms link FeNO data to electronic health records, we’re moving toward smarter, more personalized asthma care.
For now, if you’ve got asthma that’s hard to control, ask your doctor: “Could FeNO testing help us understand what’s really going on?” It might be the simplest test you’ve ever had-with the biggest impact.
What does a high FeNO level mean for asthma?
A high FeNO level (25 ppb or higher in adults, 20 ppb in children) means there’s active type 2 inflammation in your airways, often linked to eosinophils. This suggests your asthma is driven by allergic or immune responses and is likely to respond well to inhaled corticosteroids or biologic therapies. It doesn’t confirm asthma on its own, but it strongly supports the diagnosis when combined with symptoms and lung function tests.
Can FeNO testing diagnose asthma on its own?
No. FeNO testing cannot diagnose asthma alone. It’s a biomarker for inflammation, not a diagnostic test for the disease. Many people with asthma have normal FeNO levels, especially if their asthma isn’t type 2-driven. Conversely, people with allergies or eosinophilic bronchitis can have high FeNO without having asthma. Diagnosis always requires a full clinical picture: symptoms, lung function, medical history, and sometimes other tests.
How often should FeNO testing be done?
For most people on maintenance asthma therapy, FeNO testing is recommended every 3 to 4 months. More frequent testing-every 4 to 8 weeks-is advised when adjusting medications, starting a new biologic, or after a flare-up. The goal is to track trends over time, not rely on a single number. Your doctor will decide the schedule based on how well your asthma is controlled.
Why might my FeNO result be low even if I have asthma?
Low FeNO doesn’t mean you don’t have asthma. It means your asthma isn’t driven by type 2 inflammation. This can happen in non-allergic asthma, exercise-induced asthma, or asthma triggered by pollution or stress. Smoking, recent steroid use, or even poor test technique can also lower FeNO readings. If your symptoms persist despite low FeNO, your doctor will look for other causes and treatment options.
Is FeNO testing covered by insurance?
Coverage varies. Medicare in the U.S. covers FeNO testing when used for asthma management under CPT code 95012. Many private insurers cover it too, but some require prior authorization or deny it as “not medically necessary.” In the UK, NICE guidelines ensure wider NHS access. If denied, ask your doctor to submit a letter explaining how your uncontrolled symptoms and frequent exacerbations justify the test. Many appeals are approved with proper documentation.





Chris Taylor
November 29, 2025 AT 11:33I had no idea this test even existed until my pulmonologist suggested it last year. I was on three inhalers and still waking up gasping. One minute of blowing into a tube and suddenly my doctor knew exactly what was wrong. No more guessing. FeNO showed my inflammation was still sky-high even when I felt 'fine'. Switched to a biologic and I haven't had a flare-up in 14 months. Best 10 seconds of my life.
Melissa Michaels
November 30, 2025 AT 11:02FeNO is a valuable biomarker but it's not a standalone diagnostic tool. The literature is clear that it only detects type 2 inflammation and misses non-eosinophilic asthma entirely. Relying on it alone can lead to mismanagement. Always correlate with clinical history spirometry and symptom diaries. It's an adjunct not a replacement. Many clinicians still overestimate its diagnostic power.
Nathan Brown
December 2, 2025 AT 09:40It's wild when you think about it. We're measuring a molecule our bodies make to signal inflammation and turning it into a number on a screen. Nitric oxide was once just a pollutant in smog now it's a window into our lungs. Science is poetic like that. We used to rely on stethoscopes and guesswork now we can see the invisible fire inside the airways. It's not magic but it feels like it. Makes you wonder what other quiet signals our bodies are sending that we're just learning to listen to.
Olivia Currie
December 3, 2025 AT 12:54OMG I JUST GOT MY FE NO RESULTS AND THEY WERE 42 PPB!! I THOUGHT I WAS JUST A BAD ASTHMA PATIENT BUT MY DOCTOR SAID MY LUNGS WERE ON FIRE!! I WAS ON A BIOLGIC WITHIN A WEEK AND NOW I CAN RUN UP THE STAIRS WITHOUT DYING!! THIS TEST CHANGED MY LIFE!!
Curtis Ryan
December 4, 2025 AT 19:04so i got my fe no test done and it was 28 and my doc said i need a biologic but i was like wait i dont even have money for my inhalers how am i gonna afford this 30k drug?? also why does my insurance say no?? this is insane
Rajiv Vyas
December 6, 2025 AT 01:45fe no testing is just another way for big pharma to make money. they invented this test so they can sell you expensive biologics. the real cause of asthma is vaccines and 5g towers. my neighbor had high fe no and he never even got vaccinated. coincidence? i think not. also why do they only test adults over 25? they're hiding something
Astro Service
December 7, 2025 AT 02:25we dont need some fancy tube test to know if your lungs are bad. back in my day we just used our lungs and if you couldnt breathe you were weak. this is why america is soft. we used to treat asthma with cigarettes and coffee. now we need a phone app and a $300 device. this is why we lost the space race.
DENIS GOLD
December 8, 2025 AT 03:23oh wow so now we're measuring nitric oxide like it's some kind of magic spell? next they'll be testing your aura for asthma. this is what happens when you let PhDs with lab coats run medicine. my grandpa had asthma for 60 years and never saw a fe no machine. he just smoked and drank whiskey and lived to 87. this is why medicine is broken.
Ifeoma Ezeokoli
December 8, 2025 AT 07:49as someone from nigeria where we dont even have reliable access to inhalers i just want to say thank you for sharing this. i wish more doctors here knew about fe no. maybe one day this tech will be affordable and available everywhere. its not just about money its about dignity. everyone deserves to know what's happening inside their body. i hope this changes.
Sachin Agnihotri
December 10, 2025 AT 03:14Wait, so if you smoke, your FeNO drops by 30-50%? That’s a huge confounder… So if someone smokes and has asthma, they might get a false negative? That’s… problematic. And what about vaping? Does that affect it too? I think we need way more research on environmental variables. Also, is this test validated across all ethnic groups? I’m not convinced.
Pawittar Singh
December 10, 2025 AT 22:19Bro this is the future! I got my own FeNO device for $299 and test myself every week now. My doctor loves it. I send him the graph every Monday. Last month my levels spiked right before my period - turns out hormones affect inflammation too! Now I adjust my meds based on trends. Life is good. 🙌
Josh Evans
December 12, 2025 AT 21:19My kid did the test at school last year. He’s 7. Didn’t even cry. Just blew into the tube like a balloon. Got his number, doctor adjusted his inhaler, and now he plays soccer without stopping. I wish we had this when I was a kid.
Allison Reed
December 13, 2025 AT 20:41My FeNO dropped from 45 to 18 after switching to a new steroid. I didn’t feel any different at first - but the numbers told the truth. That’s the power of this test. It doesn’t lie. If your doctor isn’t using it, ask why.