When a patient walks into your office with a prescription for a brand-name drug, and you know a generic version is available, what do you do? For many providers, it’s not just about saving money-it’s about understanding what actually works in real life. Generic medications aren’t just cheaper copies. They’re rigorously tested, FDA-approved, and used by millions every day. But behind the statistics are real stories-from patients who swear their seizure control vanished after switching, to others who finally started taking their blood pressure pill because it now costs $4 instead of $40.
It’s Not Just About Cost-It’s About Trust
Providers don’t resist generics because they’re skeptical of science. The science is solid. The FDA requires generics to match brand-name drugs in active ingredients, strength, dosage form, and bioequivalence. That means the drug gets into the bloodstream at the same rate and amount. In 90% of cases, this works perfectly. But trust doesn’t come from data sheets. It comes from experience. Take antiepileptic drugs. A 2020 study in Frontiers in Drug Safety and Regulation found that neurologists overwhelmingly avoid automatic substitution for drugs like lamotrigine or levetiracetam. Why? Because even small changes in blood levels can trigger seizures in patients who were stable for years. One provider in Ohio shared a case: a 28-year-old woman with well-controlled epilepsy had three breakthrough seizures in six weeks after her pharmacy switched her from brand Lamictal to a generic. She didn’t report any side effects-just sudden, unexplained seizures. When switched back to the brand, her seizures stopped. That’s not theory. That’s clinical reality.Where Generics Shine: Statins, Blood Pressure, and Beyond
But not all drugs are created equal. For most common medications, generics are a win-win. Statins like atorvastatin, ACE inhibitors like lisinopril, and antidepressants like sertraline have decades of real-world use with no meaningful difference in outcomes. A 2019 JAMA Internal Medicine study tracked over 10 drugs with both brand and generic versions and found no difference in hospitalizations, emergency visits, or treatment discontinuation. For patients on these drugs, switching to generics often improves adherence simply because they can afford them. One primary care clinic in rural Alabama tracked 427 patients switched from brand-name atorvastatin to generic. Within six months, medication possession ratio jumped from 68% to 89%. No increase in cholesterol spikes. No rise in heart attacks. Just more people taking their pills. That’s the power of affordability. When a patient’s out-of-pocket cost drops from $120 to $8, compliance isn’t just better-it’s predictable.The Hidden Risk: Narrow Therapeutic Index Drugs
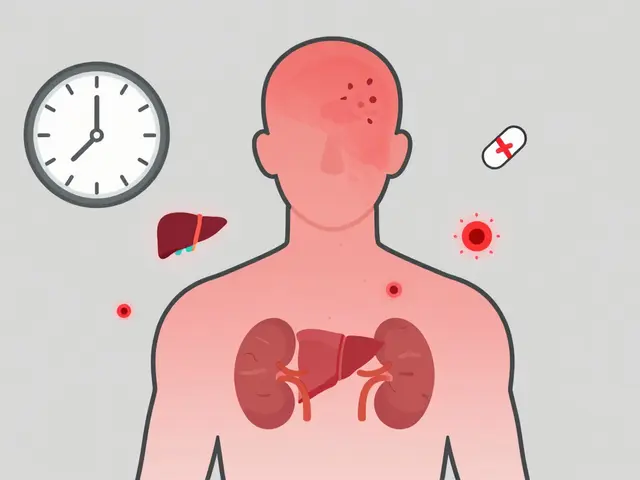
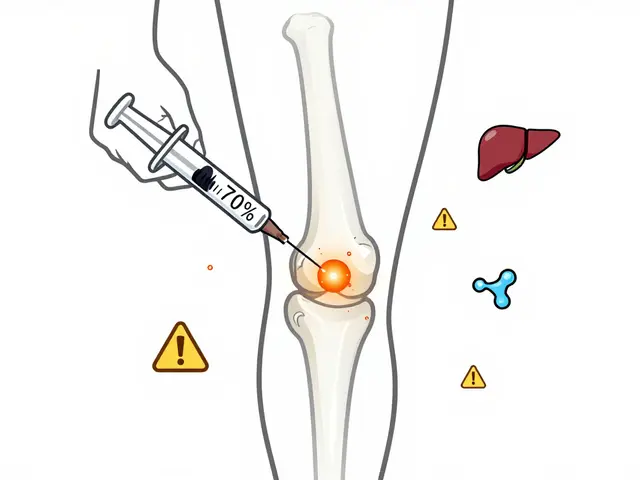
Some drugs live in a tight window. Too little, and the disease returns. Too much, and the patient gets sick or worse. These are called narrow therapeutic index (NTI) drugs. They include warfarin, levothyroxine, cyclosporine, and phenytoin. Providers treat these with extreme caution. A 2015 systematic review found that nearly 75% of studies on generic substitution focused on NTI drugs-because that’s where the risk is highest. One endocrinologist in Minnesota recounted switching a thyroid patient from brand Synthroid to a generic. Her TSH levels, stable at 2.1 for two years, jumped to 7.8 within six weeks. She felt exhausted, gained weight, and her cholesterol climbed. After switching back, everything normalized. The FDA’s own data shows that even small differences in absorption can matter here. That’s why many providers write “dispense as written” on these prescriptions-and why some states require explicit patient consent before substitution.
Authorized Generics: The Bridge Between Brand and Generic
Then there’s the lesser-known option: authorized generics. These are the exact same pills as the brand-name drug, just sold without the brand label. Made by the original manufacturer, they’re often priced like generics. For providers who want to preserve consistency but reduce cost, this is the sweet spot. A patient on Concerta (brand-name methylphenidate) was switched to a regular generic and began reporting reduced focus and increased irritability. The FDA investigated and found two generic versions had significantly more “lack of effect” complaints. They downgraded those generics from AB to BX rating-meaning they’re no longer considered therapeutically equivalent. But when the patient was switched to the authorized generic (made by Janssen, the original maker), symptoms disappeared. No change in the pill-just the label. That’s the kind of insight that changes how providers think about substitution.State Laws Are a Patchwork-And It Confuses Everyone
You can’t talk about generic substitution without talking about the mess of state laws. In 19 states, pharmacists can switch a brand to generic without telling the patient. In 7 states and Washington, D.C., they must get written consent. In 31 states, patients must be notified-but not always in a way they understand. Some pharmacies just slap a sticker on the bottle. Patients think they’re getting a different drug. A 2024 survey in Greece showed that patients who had a direct conversation with their provider about generics were far more likely to accept them. But in the U.S., many providers don’t have the time. Electronic health records now include therapeutic equivalence ratings (AB, BX), but not all systems display them clearly. A provider in Texas shared that her EHR flagged a generic for warfarin as “AB,” but the pharmacy substituted anyway. The patient’s INR spiked. She didn’t know the pill changed. The provider didn’t know it happened until the lab result came back.What Providers Are Doing Differently Now
The best providers aren’t just prescribing generics-they’re managing the transition. They’re:- Starting with low-risk drugs first: statins, metformin, SSRIs
- Documenting the brand and generic used in the chart
- Asking patients: “Have you taken this drug before? Did it work?”
- Monitoring labs closely after switches for NTI drugs
- Using authorized generics when available for patients who’ve had bad experiences
- Training staff to explain that a different-looking pill isn’t a different drug
The Bigger Picture: Why This Matters
In 2023, generics made up 90% of prescriptions in the U.S. but only 23% of drug spending. That’s over $130 billion saved annually. That money keeps people on their meds, prevents hospitalizations, and reduces the burden on the system. But savings mean nothing if patients stop taking their pills because they’re confused, scared, or had a bad experience. The goal isn’t to push generics at all costs. It’s to match the right drug to the right patient at the right time. For most, generics are perfect. For a small but critical group, they’re not. The provider’s job isn’t to choose between brand and generic-it’s to choose the best path for each person.What’s Next?
The FDA is now using real-world data from the Sentinel Initiative to track outcomes after substitution-not just lab results, but ER visits, hospital stays, and patient reports. Machine learning models are being tested to predict who’s likely to have trouble switching based on age, comorbidities, and past adherence. And with the Inflation Reduction Act pushing Medicare to favor generics even more, providers will need to be even more intentional. The future of generics isn’t about cost alone. It’s about precision. It’s about communication. It’s about listening to patients-and to the data.Are generic medications as effective as brand-name drugs?
Yes-for most medications, generics are just as effective. The FDA requires them to deliver the same amount of active ingredient into the bloodstream at the same rate as the brand-name version. Studies involving over 10 common drugs found no difference in hospitalizations, emergency visits, or treatment failure. However, for narrow therapeutic index drugs like warfarin, levothyroxine, or antiepileptics, even small differences can matter. Providers often recommend staying on the same version-brand or generic-once a stable dose is found.
Why do some patients have problems after switching to generics?
Most patients don’t. But for some, especially those on drugs with a narrow therapeutic index, even minor differences in how the drug is absorbed can trigger side effects or loss of control. In epilepsy, switching from brand to generic lamotrigine has been linked to breakthrough seizures in some patients. In thyroid patients, switching generics can cause TSH levels to fluctuate. These aren’t due to poor quality-they’re due to subtle differences in formulation. That’s why providers often avoid automatic substitution for these drugs and prefer to keep patients on the same version once it’s working.
What’s the difference between a generic and an authorized generic?
A regular generic is made by a different company, using the same formula as the brand. An authorized generic is made by the original brand-name manufacturer, but sold without the brand label. It’s physically identical to the brand drug-same ingredients, same factory, same packaging (except for the name). Authorized generics are often used when patients have had trouble with regular generics, or when providers want to ensure consistency without the brand price.
Can pharmacists switch my brand drug to a generic without telling me?
It depends on your state. In 19 states, pharmacists can substitute generics without notifying you. In 7 states and Washington, D.C., they must get your consent. In 31 states, you must be notified, but the notification isn’t always clear-sometimes it’s just a sticker on the bottle. Always ask if your prescription was switched, especially if you’re on a drug for epilepsy, thyroid, or blood thinning. Your provider can write “dispense as written” on the prescription to prevent automatic substitution.
Why do some generics look different from others?
Generic drugs can come from different manufacturers, and each uses different inactive ingredients-like fillers, dyes, or coatings. That’s why pills might change color, shape, or size from one refill to the next. But the active ingredient is the same. The FDA requires this. If you’re confused by the change, ask your pharmacist. It doesn’t mean the drug is weaker or different-it just means the manufacturer changed. For patients on sensitive medications, switching manufacturers can sometimes cause issues, which is why consistency matters.
Should I avoid generics because they’re cheaper?
No. Price doesn’t indicate quality when it comes to FDA-approved generics. The FDA inspects manufacturing facilities for generics the same way it does for brand-name drugs. The reason generics are cheaper is because they don’t need to repeat expensive clinical trials. They only need to prove they work the same way in the body. Studies show generics save billions annually and improve adherence because patients can afford them. Avoiding generics because they’re cheap is like avoiding a reliable used car because it’s not a luxury brand.
How do I know if a generic is rated as therapeutically equivalent?
The FDA publishes the Orange Book, which lists all approved drugs and their therapeutic equivalence ratings. Look for “AB” rating-it means the generic is considered equivalent to the brand. “BX” means it’s not rated as equivalent, often due to concerns about absorption or effectiveness. Your pharmacist or provider can check this. Some electronic health records now flag these ratings automatically. If you’re on a critical medication and your generic changes, ask if it still has an AB rating.



Sarah Little
January 4, 2026 AT 16:39Let’s be real-the bioequivalence thresholds for generics are laughably loose. AB-rated doesn’t mean identical, it means ‘close enough for regulatory paperwork.’ I’ve seen TDM data where generics fluctuate 15-20% in Cmax vs. brand, and in NTI drugs? That’s clinically significant. The FDA’s 80-125% AUC range is a statistical loophole, not a clinical guarantee. Providers who don’t track serum levels post-switch are gambling with patient outcomes.
innocent massawe
January 5, 2026 AT 10:11in my country, generics are the only option-and people live longer because of it. 🌍❤️ no one here has seizures from switching meds. maybe it’s about how we train pharmacists, or how we talk to patients. not all problems are in the pill. sometimes, it’s in the fear.
Tru Vista
January 6, 2026 AT 11:39NTI drugs? Yeah. But 90% of Rx’s aren’t NTI. Stop overcomplicating. Statins? Metformin? Sertraline? Generics work. Period. If your patient has a seizure after switching lamotrigine, maybe they weren’t stable to begin with. Or maybe you didn’t monitor. The data says 90% work fine. Stop letting outliers dictate policy.
JUNE OHM
January 6, 2026 AT 14:55THE FDA IS IN BED WITH BIG PHARMA. 🚨 They let generics slide because they’re paid off. Look at the authorized generics-why do the SAME companies make the brand AND the ‘generic’? It’s a scam. They charge you $40 for the brand, then sell you the exact same pill for $4 under a different label. You’re being played. And they call it ‘savings’? No. It’s price gouging with a new name.
Philip Leth
January 7, 2026 AT 16:01Man, I work in a clinic in rural Texas. We switched 300 people to generics last year. Only 3 came back saying ‘this ain’t right.’ One had a bad reaction to a generic phenytoin-totally legit. But the other two? They just didn’t like the color. One guy thought the blue pill meant ‘it’s weaker.’ We made a handout with pics. Now he takes it fine. It’s not the drug. It’s the story we tell.
Angela Goree
January 8, 2026 AT 16:57State laws? Why are we letting pharmacists make medical decisions?!?!?!!?!!? The doctor prescribes. The pharmacist dispenses. That’s it. No substitutions without consent. No stickers. No ‘you’re fine.’ If I write ‘dispense as written,’ I expect it to be followed. Not because I’m controlling-I’m protecting. This isn’t a grocery store. This is someone’s brain, heart, thyroid. Don’t you dare swap it without asking.
Tiffany Channell
January 8, 2026 AT 21:14Everyone’s acting like generics are this magical solution. But the data is cherry-picked. You cite JAMA? What about the 2021 NEJM paper showing higher discontinuation rates with generics in bipolar patients? And don’t get me started on the lack of post-market surveillance. The FDA doesn’t track real-world outcomes-only pre-approval bioequivalence. That’s like saying two cars are the same because they both have four wheels. You’re not a doctor-you’re a statistician with a clipboard.
Angela Fisher
January 10, 2026 AT 06:21Have you ever seen what’s in these generics?? I mean, REALLY looked? Fillers. Dyes. Binders. Some of them have traces of heavy metals-yes, I’ve seen the FDA inspection reports. And the companies? They rotate factories every few months. One batch is fine, next one? Your TSH goes nuts. And the FDA? They only test one batch per year. One. And you think that’s enough? No. This is why people get sick. It’s not the active ingredient-it’s the junk they hide inside. And they call it ‘safe’? Please. I’ve seen patients collapse after switching. No one listens. They just say ‘it’s the same.’ It’s NOT the same. The pill looks different. It tastes different. It FEELS different. And your body knows.
Neela Sharma
January 10, 2026 AT 18:15Medicine is not just chemistry-it is trust. A pill is not just molecules. It is the quiet promise between a healer and a human. When the color changes, the shape shifts, the name vanishes-it shakes that promise. Some patients don’t need science. They need to feel safe. And sometimes, safety is not in the active ingredient-but in the familiar weight of the pill in their palm. So yes, for some, the brand is worth the cost. Not because it works better. But because it lets them breathe.