Behavior Disorder Medication Selector
Select Your Primary Concerns
Answer these questions to identify appropriate medication options for behavior disorders.
Based on your responses, these medication classes may be appropriate for your situation:
When it comes to behavior disorder medication, the options can feel overwhelming - especially with new drugs hitting the market each year. This guide walks you through the most common medication classes, how they work, and practical tips for choosing the right treatment for kids and adults dealing with behavior‑related conditions.
Key Takeaways
- Stimulants remain the first‑line choice for ADHD but aren’t the only option.
- Non‑stimulants, atypical antipsychotics, SSRIs, and mood stabilizers each target different symptom clusters.
- Age, co‑existing conditions, and side‑effect profiles drive medication selection.
- Regular monitoring and clear communication with clinicians boost safety and effectiveness.
Behavior disorder medication is a pharmacological treatment designed to reduce impulsivity, aggression, mood swings, or hyperactivity associated with psychiatric and neurodevelopmental disorders. It covers a range of drug families, from stimulants for ADHD to antipsychotics for severe aggression. While medication isn’t a cure, it can create a stable platform for therapy, schooling, and daily life.
Understanding Common Behavior Disorders
Before picking a pill, you need to know what you’re treating. The most frequently diagnosed behavior‑related conditions include:
- Attention‑deficit/hyperactivity disorder (ADHD): persistent inattention, hyperactivity, and impulsivity.
- Oppositional defiant disorder (ODD): pattern of hostile, disobedient, and defiant behavior toward authority figures.
- Autism spectrum disorder (ASD): includes sensory sensitivities and repetitive behaviors that can cause distress.
- Conduct disorder: severe aggression, rule‑breaking, and lack of empathy that can progress to criminal activity.
These disorders often overlap, and medication choices reflect the dominant symptoms.
How Medications Work
All behavior disorder medication aims to modify neurotransmitter activity in the brain. Think of neurotransmitters as messengers that influence attention, mood, and impulse control. Different drug classes target different messengers - dopamine, norepinephrine, serotonin, or glutamate - producing varied therapeutic effects.

Major Medication Classes
Stimulant Medication
Stimulant medication boosts dopamine and norepinephrine levels, sharpening focus and reducing hyperactivity. They’re the go‑to for ADHD and have the fastest onset (30‑60 minutes).
- Common brands: Methylphenidate (Ritalin, Concerta), Amphetamine‑based (Adderall, Vyvanse).
- Typical side‑effects: appetite loss, sleep trouble, mild anxiety.
Non‑Stimulant Medication
Non‑stimulant medication modulates norepinephrine or serotonin without the rapid dopamine surge. Useful when stimulants cause intolerable side‑effects or when there’s a co‑existing anxiety disorder.
- Atomoxetine (Strattera) - norepinephrine reuptake inhibitor.
- Guanfacine (Intuniv) and Clonidine (Kapvay) - alpha‑2 agonists that improve impulse control.
Atypical Antipsychotic
Atypical antipsychotic blocks dopamine D2 receptors and modulates serotonin, reducing aggression and severe mood swings. Often added for ODD, conduct disorder, or ASD‑related irritability.
- Risperidone (Risperdal) and Aripiprazole (Abilify) are FDA‑approved for irritability in ASD.
- Metabolic side‑effects (weight gain, glucose changes) require regular labs.
Selective Serotonin Reuptake Inhibitor (SSRI)
Selective serotonin reuptake inhibitor (SSRI) increases serotonin availability, easing anxiety, obsessive‑compulsive traits, and mood dysregulation. Beneficial when anxiety or depression fuels disruptive behavior.
- Fluoxetine (Prozac), Sertraline (Zoloft), and Escitalopram (Lexapro) are common choices.
- Watch for activation (restlessness) in children; start low and titrate slowly.
Mood Stabilizer
Mood stabilizer dampens extreme mood swings by targeting calcium channels or glutamate pathways. Used for bipolar‑type presentations or severe emotional lability.
- Lithium, Valproate (Depakote), and Lamotrigine (Lamictal).
- Requires blood level monitoring and renal/hepatic checks.
Alpha‑2 Agonist
Alpha‑2 agonist reduces norepinephrine release, calming the nervous system and improving executive function. Often combined with stimulants to smooth out emotional spikes.
- Clonidine (Kapvay) - oral form for daytime control.
- Guanfacine (Intuniv) - longer half‑life, once‑daily dosing.
Comparison of Medication Classes
| Class | Primary Uses | Common Brands | Typical Onset | Key Side‑effects |
|---|---|---|---|---|
| Stimulant | ADHD core symptoms | Ritalin, Concerta, Adderall, Vyvanse | 30‑60 min | Appetite loss, insomnia, increased heart rate |
| Non‑stimulant | ADHD when stimulants unsuitable; anxiety‑linked impulsivity | Strattera, Intuniv, Kapvay | 1‑2 weeks | Dry mouth, fatigue, low blood pressure |
| Atypical antipsychotic | Severe aggression, irritability in ASD/ODD | Risperdal, Abilify | 1‑2 weeks | Weight gain, metabolic syndrome, sedation |
| SSRI | Anxiety, OCD, mood dysregulation | Prozac, Zoloft, Lexapro | 4‑6 weeks | GI upset, activation, rare serotonin syndrome |
| Mood stabilizer | Bipolar‑type mood swings, severe lability | Lithium, Depakote, Lamictal | 1‑2 weeks (adjusted) | Thyroid, kidney, liver monitoring needed |
| Alpha‑2 agonist | Impulse control, adjunct to stimulants | Kapvay, Intuniv | 1‑2 weeks | Drowsiness, dry mouth, hypotension |

Choosing the Right Medication: Practical Factors
Everyone’s brain chemistry is unique, so clinicians weigh several variables before writing a prescription:
- Age and developmental stage - younger children may need lower doses or non‑stimulants to avoid growth impact.
- Dominant symptoms - hyperactivity vs. aggression vs. anxiety dictates the drug class.
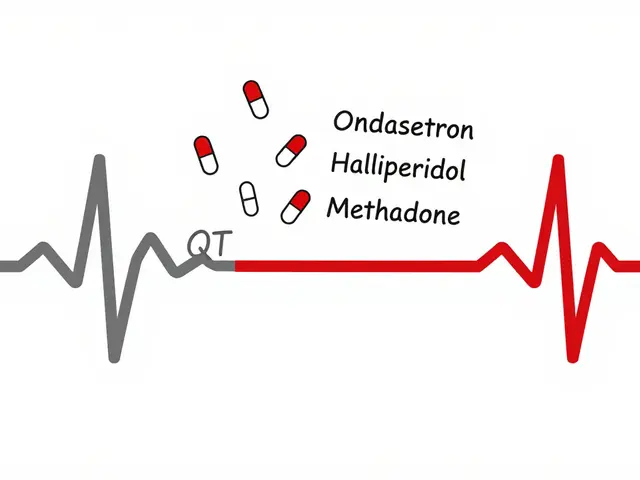
- Co‑existing conditions - anxiety, depression, seizure history, or cardiac issues narrow choices.
- Side‑effect tolerance - families prioritize sleep, appetite, or weight concerns differently.
- Monitoring logistics - blood work for lithium or metabolic panels for antipsychotics require clinic visits.
Shared decision‑making boosts adherence. A typical workflow looks like:
- Baseline assessment (rating scales, physical exam, labs if needed).
- Discuss options, benefits, and risks in plain language.
- Start low, titrate slowly - most guidelines recommend a 4‑week titration window.
- Schedule follow‑up at 1, 4, and 12 weeks to gauge efficacy and side‑effects.
- Adjust dose or switch class based on response.
Checklist for Patients, Parents, and Clinicians
- Confirm the exact diagnosis and symptom targets.
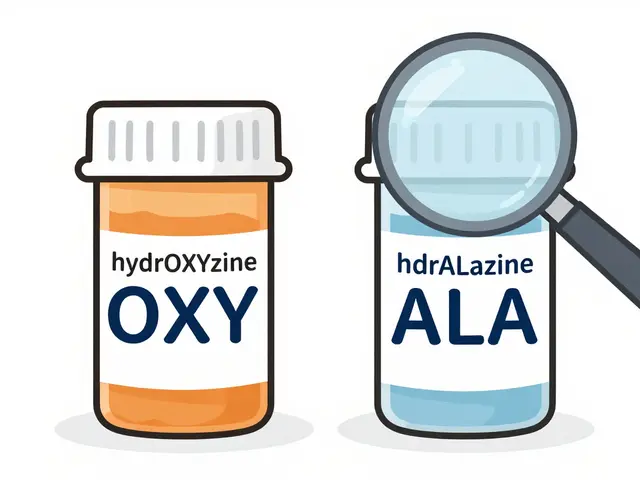
- Review any current meds for drug‑drug interactions.
- Ask about dosage form (tablet, chewable, extended‑release) that fits daily routine.
- Set clear, measurable goals (e.g., “stay seated for 15 min during class”).
- Document side‑effects daily in a simple log.
- Plan for regular labs if using antipsychotics, mood stabilizers, or high‑dose stimulants.
- Discuss behavioral therapy or coaching as a companion to meds.
Frequently Asked Questions
Can a child take stimulant medication long‑term?
Yes, many children stay on stimulants for years. Regular growth monitoring and periodic breaks (e.g., “drug holidays” during summer) help manage potential side‑effects.
Are antipsychotics safe for non‑psychotic behavior issues?
When prescribed at low doses for aggression or irritability, atypical antipsychotics are considered safe, but they demand monthly metabolic labs and close weight monitoring.
What’s the difference between guanfacine and clonidine?
Both are alpha‑2 agonists, but guanfacine has a longer half‑life and fewer sleep‑related side‑effects, making it a preferred once‑daily option for ADHD adjunct therapy.
Do SSRIs cause hyperactivity in kids?
A subset of children experience activation-restlessness, insomnia, or increased impulsivity-especially during the first weeks. Starting at the lowest dose and titrating slowly usually mitigates this.
How often should labs be drawn for lithium?
Initially weekly until stable, then every 3‑6 months for serum lithium level, thyroid function, and renal panels.
Medication isn’t a magic bullet, but the right behavior disorder medication can reduce daily chaos, improve learning, and give families breathing room. Pairing drugs with behavioral interventions, consistent routines, and regular follow‑up creates the best chance for lasting improvement.



Dan Danuts
October 23, 2025 AT 15:33Hey folks, great rundown! 🎉 If you're thinking about starting a stimulant, remember a low‑dose trial can reveal how your kid handles side‑effects before you go full‑blast. It also helps to keep a simple behavior log-just note the hour meds were taken and any appetite changes. Pairing the med with a short, structured activity after school often boosts the positive effects. And don’t forget to celebrate small wins; they build momentum for bigger improvements.
Dante Russello
November 1, 2025 AT 16:36Indeed, the low‑dose approach, while seemingly simple, actually provides a crucial data point; it allows clinicians to calibrate pharmacodynamics, monitor tolerability, and adjust titration schedules accordingly. Moreover, a daily log-especially one that timestamps medication intake, meals, and sleep-serves as an empirical baseline; it facilitates nuanced discussions with prescribers, and, ultimately, promotes shared decision‑making.
Scott Ring
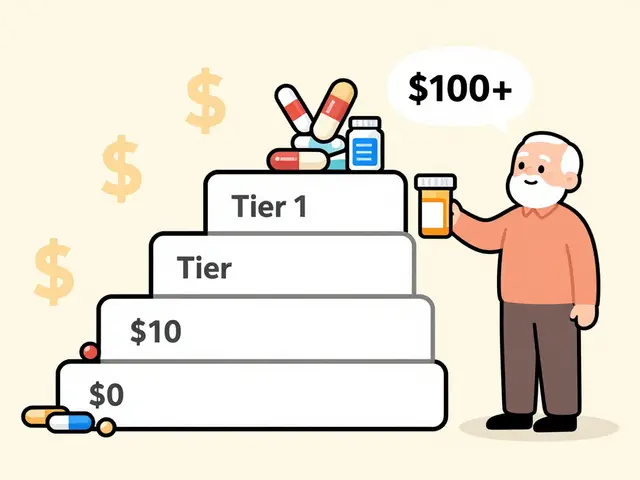
November 10, 2025 AT 18:40Just a heads‑up from a cultural perspective: some families prefer chewable or liquid formulations because kids might resist pills. Those options can be especially handy during school trips or summer camps. Also, keep an eye on insurance formularies; they sometimes favor one brand over another, which can affect out‑of‑pocket costs.
Shubhi Sahni
November 19, 2025 AT 20:43When selecting a medication, it's essential to align the drug's onset profile with the child's daily routine; for instance, an extended‑release stimulant taken in the morning can cover school hours without midday dosing. Additionally, consider non‑pharmacologic supports like classroom accommodations-they amplify the medication's benefits. Regular check‑ins with the pediatrician, every 3‑4 weeks initially, ensure any emerging side‑effects are caught early.
Danielle St. Marie
November 28, 2025 AT 22:46Honestly, if you're not reading the fine print on metabolic side‑effects, you're setting yourself up for disappointment. 🤦♀️ Choose wisely!
keerthi yeligay
December 8, 2025 AT 00:50Do you check labs before starting.
Peter Richmond
December 17, 2025 AT 02:53For atypical antipsychotics, baseline fasting glucose and lipid panels are a must before initiation. Follow‑up labs should be drawn at 3 months, then semi‑annually. This schedule helps catch metabolic shifts early, preserving both physical health and therapeutic efficacy.
sara fanisha
December 26, 2025 AT 04:56Super helpful guide! I love the tip about “drug holidays” during summer-it really takes the pressure off parents. Also, the reminder to set measurable goals, like “stay seated for 15 minutes,” makes tracking progress way easier. Keep the positivity coming!
Jinny Shin
January 4, 2026 AT 07:00Ah, the theater of pharmacology unfolds before us, each molecule a protagonist in the drama of the mind! The stimulant, that mercurial spark, darts across synapses, urging dopamine to pirouette, while the non‑stimulant takes a measured bow, soothing norepinephrine with a gentle hand. One can almost hear the hush as the atypical antipsychotic enters, its cloak of dopamine blockade casting shadows upon aggression, yet whispering promises of calm. Meanwhile, the SSRI, that lyrical poet, weaves serotonin verses that soften the edges of anxiety, though sometimes it stirs a restless chorus in the young. Mood stabilizers stand as stoic guardians, their calcium‑channel guardianship keeping emotional tides from crashing. And let us not neglect the humble alpha‑2 agonist, the quiet understudy, ready to smooth the erratic spikes of impulse. Each class, a cast of characters, demands a director-our clinicians-to orchestrate timing, dosage, and monitoring. The first act, baseline assessment, is the prologue where scales are weighed and labs drawn, setting the stage for informed choice. In the second act, shared decision‑making, families and physicians exchange soliloquies of risk and reward, crafting a script tailored to the child's unique narrative. The third act, titration, unfolds over weeks, a cautious crescendo where doses rise like a dawning sun, illuminating efficacy while watching for side‑effects lurking in the wings. As the curtain rises on follow‑up visits, data from behavior logs and lab results inform the final tableau-whether to sustain, adjust, or rewrite the role entirely. And ever present, the supporting cast of therapy, routine, and education, their subtle harmonies enriching the pharmacologic melody. In this grand production, patience is the director's cue, allowing each drug to reveal its true performance. Remember, no single agent can claim the starring role; it is the ensemble that delivers the encore of stability and growth. So let us applaud the science, honor the art, and sit with awe as the story of behavior disorder treatment continues to evolve.
deepak tanwar
January 13, 2026 AT 09:03While the previous exposition is undeniably poetic, it glosses over pragmatic concerns. Not all families can afford the luxury of prolonged titration periods; insurance barriers often dictate which agents are truly accessible. Moreover, the suggestion to rely heavily on behavioral logs presumes consistent caregiver engagement-a luxury not everyone possesses. We must also question the safety narrative surrounding atypical antipsychotics; their metabolic sequelae can be profound, demanding vigilant monitoring that many clinics cannot provide. Thus, a more grounded, cost‑aware approach is essential.
Abhishek Kumar
January 22, 2026 AT 11:06The guide is solid, though it could trim some repetition. Overall, a decent snapshot for newcomers.
Heather ehlschide
January 31, 2026 AT 13:10To expand on the concerns raised, it’s worth noting that baseline metabolic panels can be streamlined using a single fasting draw, reducing appointment burden. When cost is an issue, generic formulations of stimulants and certain non‑stimulants often provide comparable efficacy with lower copays. Additionally, telehealth follow‑ups can supplement in‑person labs, ensuring continuity without excessive travel. Ultimately, aligning therapeutic goals with practical constraints fosters sustainable treatment.