Constipation isn’t just about not going to the bathroom often-it’s about struggling to pass hard, dry stools, feeling like you haven’t fully emptied your bowels, or needing to strain for minutes without success. If this happens three times a week or less, it’s medically classified as constipation. Around one in three people in clinical settings experience it, and in the U.S. alone, over 2.5 million visits to doctors each year are for this issue. It’s not a minor annoyance; it’s a common, often misunderstood problem that can drag on for months or years if not handled right.
Why Does Constipation Happen?
It’s easy to blame diet, but constipation has many layers. At its core, it happens when your colon absorbs too much water from waste, turning it into hard, stubborn stools. Normally, food moves through your digestive tract in 24 to 72 hours. When that process slows down, you’re at risk. There are two main categories: primary (functional) and secondary. Primary constipation means there’s no obvious disease causing it-it’s often tied to lifestyle. Not eating enough fiber (most people get only 15g a day, but you need 25-30g), not drinking enough water (less than 1.5-2 liters), or sitting too much can all trigger it. Even ignoring the urge to go can train your body to ignore signals over time. Secondary constipation comes from other conditions or medications. Opioids cause constipation in up to 95% of users. Calcium channel blockers like verapamil and tricyclic antidepressants are common culprits too. Medical conditions like diabetes (affecting nearly 60% of patients), hypothyroidism, Parkinson’s disease, and multiple sclerosis are strongly linked. Women are more likely to experience it, especially as they age-prevalence jumps from 15% in your 20s to over 34% by your 60s.Types of Constipation You Might Have
Not all constipation is the same. Knowing the type helps you pick the right fix.- Normal transit constipation (60% of cases): Your colon moves stool at a normal speed, but you still strain, feel incomplete, or pass hard stools. This is often tied to pelvic floor issues or ignoring urges.
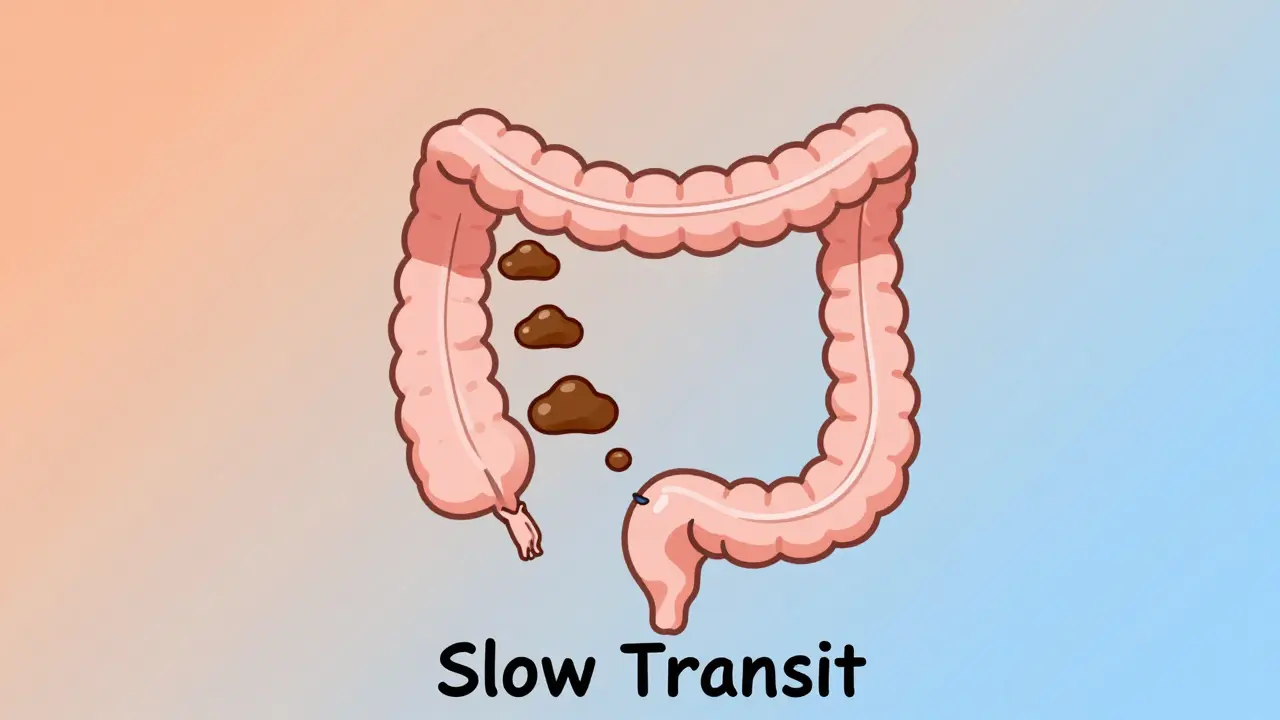
- Slow transit constipation (15-30%): Stool moves too slowly through the colon-sometimes taking over 72 hours. This is common in older adults and people with diabetes.
- Defecatory disorders (20-50%): Your pelvic floor muscles don’t relax properly when you try to go. You might push hard but nothing comes out. This is often diagnosed with a balloon expulsion test or anorectal manometry.
- Refractory constipation (15-20%): You’ve tried at least one laxative and nothing works. This often needs specialist care.
Laxatives: What Works and What Doesn’t
Laxatives are often the first line of defense-but not all are created equal. Here’s what the data says.- Bulk-forming laxatives (psyllium, methylcellulose): These absorb water and swell up to create softer, bulkier stools. They work well for normal transit constipation, but only if you drink enough water-8 ounces per dose or you risk blockage. About half of users see improvement.
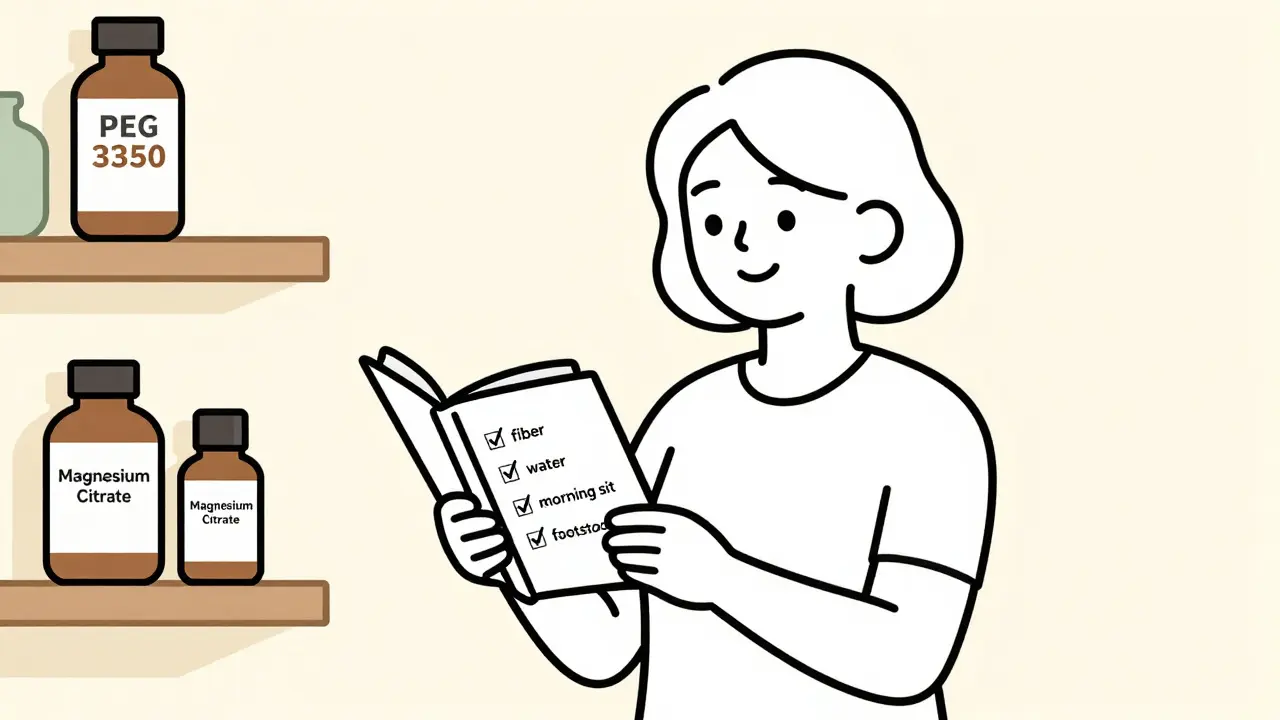
- Osmotic laxatives (PEG 3350, lactulose, magnesium hydroxide): These pull water into the colon. PEG 3350 (Miralax) is the top recommendation-65-75% effective, safe for long-term use, and gentle. It’s the first-line choice for most doctors.
- Stimulant laxatives (senna, bisacodyl): These crank up colon contractions. They work fast-often within 6-12 hours-and help 70-80% of people. But they’re not for daily use beyond 2-3 weeks. Long-term use can damage the colon’s natural movement (called cathartic colon).
- Stool softeners (docusate sodium): These are overhyped. Studies show they’re barely better than a placebo. Don’t rely on them alone.
- Prescription options (lubiprostone, linaclotide, plecanatide): For stubborn cases, these drugs activate chloride channels to increase fluid in the gut. Linaclotide helps 45-60% of patients with IBS-C. They’re expensive but life-changing for those who’ve tried everything else.
On Reddit’s r/Constipation community, users report magnesium citrate (250-350mg daily) works well for 65-70%, but 25% get diarrhea. That’s a common trade-off: relief versus side effects.
Long-Term Management: Beyond Pills
If you’re stuck on laxatives, you’re not alone. But long-term relief comes from habits, not just chemicals.- Gradually increase fiber: Jumping from 15g to 30g overnight causes bloating in 30-40% of people. Add 5g every 3-4 days. Focus on soluble fiber: oats, beans, apples, flaxseeds. It holds water and softens stool better than insoluble fiber like bran.
- Hydrate properly: For every 5g of extra fiber, drink an extra 250-500mL of water. Most people forget this. That’s why fiber sometimes makes constipation worse.
- Train your body to go: Sit on the toilet for 10-15 minutes after breakfast. That’s when your gastrocolic reflex is strongest. Don’t rush. Don’t scroll. Just sit.
- Use a footstool: Elevating your feet to a 35-degree angle (like squatting) straightens the rectum and reduces straining by 60%. A simple plastic stool works better than any pill.
- Try biofeedback: If you have pelvic floor dysfunction, this therapy retrains your muscles. Six to eight weekly sessions with a specialist lead to improvement in 70-80% of cases. It’s not quick, but it’s one of the most effective long-term fixes.
One woman in her 50s, after years of failed laxatives, got regular bowel movements with 25g of psyllium husk daily, 2 liters of water, morning coffee (to trigger the reflex), and 10 minutes of squatting each day. Within 8 weeks, she stopped needing meds.
When to Worry: Alarm Symptoms
Constipation is usually harmless. But some signs mean you need testing right away:- Unintentional weight loss of 10 pounds or more
- Rectal bleeding or dark, tarry stools
- A sudden, lasting change in bowel habits (over 6 weeks)
- Family history of colorectal cancer
- Severe abdominal pain or vomiting
The American College of Gastroenterology says these aren’t just “maybe” signs-they’re red flags. Get a colonoscopy or other tests. Constipation can be the first symptom of a tumor, especially in older adults.
Why Most People Fail at Long-Term Relief
You’ve probably tried everything. So why does it keep coming back?- Laxative dependency fears: 42% of patients worry they’ll become addicted. But osmotic laxatives like PEG don’t cause dependence. Stimulants might, but only if used daily for months.
- Unrealistic expectations: Most people expect relief in 24 hours. Osmotic laxatives take 48-72 hours. Fiber takes weeks. Patience is part of the treatment.
- Poor follow-through: 68% of people who start a high-fiber diet relapse within 3 months. It’s hard to change habits. But consistency beats intensity.
- Doctor visits that don’t help: 35% of patients say they got less than 5 minutes of advice. Constipation is often dismissed. Don’t accept that. Ask about transit time tests or biofeedback.
The Future of Constipation Care
New tools are emerging. The FDA approved tenapanor (Ibsrela) in 2022 for IBS-C, helping 45% of users get relief. The NIH is funding research into gut bacteria-people with constipation often have low levels of Bacteroides uniformis. Probiotics targeting this could be next. Researchers at Augusta University are testing smartphone apps that analyze how you push during bowel movements. Early results show 85% accuracy in spotting pelvic floor dysfunction. Imagine diagnosing a muscle issue without a probe. The bottom line? Constipation is complex, but it’s not hopeless. Most people don’t need surgery or lifelong drugs. They need the right mix of fiber, water, timing, and posture-and the patience to stick with it.How long does it take for fiber to work for constipation?
It usually takes 4-6 weeks to see steady improvement with increased fiber. Start slow-add 5g every 3-4 days-and drink plenty of water. Rushing the increase causes bloating and gas, which makes people quit. Consistency matters more than speed.
Is it safe to take laxatives every day?
Osmotic laxatives like PEG 3350 are safe for daily, long-term use. They don’t damage the colon or cause dependency. Stimulant laxatives like senna should be limited to 2-3 weeks. Using them daily for months can lead to colon muscle weakness, known as cathartic colon. Always talk to your doctor before using stimulants regularly.
Can dehydration cause constipation?
Yes. When you don’t drink enough water, your colon pulls more fluid from stool to keep your body hydrated. That leaves stools hard and dry. Aim for 1.5-2 liters daily, and add 250-500mL for every 5g of extra fiber you eat. Coffee and tea count toward your total, but avoid sugary drinks.
Why does constipation get worse with age?
As you age, your digestive system slows down. Muscle contractions in the colon weaken, pelvic floor muscles lose tone, and you may take more medications that cause constipation (like blood pressure pills or painkillers). Also, older adults often drink less water and move less. It’s not inevitable-good habits can offset it.
Do probiotics help with constipation?
Some strains show promise, especially in people with IBS-C. Bifidobacterium and Lactobacillus have helped in small studies, but results aren’t consistent. The most exciting research is targeting specific bacteria like Bacteroides uniformis, which is often low in constipated people. Probiotic supplements aren’t yet a standard treatment, but future therapies may use targeted strains.
When should I see a specialist for constipation?
See a gastroenterologist if you’ve tried lifestyle changes and osmotic laxatives for 3 months with no improvement, or if you have alarm symptoms like weight loss, bleeding, or pain. Specialists can do tests like colonic transit studies or anorectal manometry to find the root cause-especially if you have pelvic floor dysfunction or slow transit.





Stacy Thomes
January 23, 2026 AT 10:50This article just saved my life. I’ve been on laxatives for YEARS and never knew about the footstool trick. I bought a $12 plastic stool from Amazon and now I go like clockwork. No more straining. No more shame. Thank you.
Also, psyllium husk + 2 liters of water = magic. I was skeptical but now I’m obsessed.
Dawson Taylor
January 23, 2026 AT 23:46The physiological mechanisms underlying colonic transit dysfunction are elegantly delineated in this exposition. One is compelled to acknowledge the preponderance of evidence favoring osmotic agents over stimulant cathartics in chronic management paradigms. The role of pelvic floor dyssynergia remains underappreciated in primary care settings.
Oladeji Omobolaji
January 24, 2026 AT 08:01Man, I thought I was the only one struggling with this. Nigeria got same problem but nobody talks about it. We just eat more garri and pray. This post? Real talk. I’m trying the footstool tomorrow.
dana torgersen
January 25, 2026 AT 02:16I… I just… I mean, I’ve been doing everything right… fiber… water… coffee… squatting… but why… why does it still feel like my colon is made of concrete?!?!?!!? I’m so tired… I just want to go… and not feel like I’m giving birth to a brick…
Sallie Jane Barnes
January 26, 2026 AT 16:48Thank you for this comprehensive, evidence-based overview. It is rare to encounter such clarity on a topic often dismissed as trivial. The emphasis on behavioral modification over pharmaceutical dependency is both clinically sound and profoundly humane.
Susannah Green
January 27, 2026 AT 00:48For anyone still using docusate: stop. It’s a placebo with a price tag. I used to take it daily for years-wasted money. PEG 3350 is the real MVP. Also, don’t forget magnesium citrate-it’s fast, cheap, and works for most people. Just don’t overdo it or you’ll be on the toilet all day.
And yes, the footstool? Game changer. I use a stack of books. No joke.
Kerry Moore
January 27, 2026 AT 03:08I appreciate the nuance in distinguishing between transit types and the emphasis on biofeedback. Many patients are never evaluated for pelvic floor dysfunction. This level of detail deserves wider dissemination in primary care education.
Sue Stone
January 28, 2026 AT 06:12Been here. Tried everything. The only thing that worked? Walking 30 mins after dinner. No joke. Just walk. Not run. Not yoga. Just walk. My body figured it out. Weird, right?
Vanessa Barber
January 28, 2026 AT 14:15Okay but… are we sure this isn’t just a ‘sit on the toilet longer’ scam? I’ve been sitting there for 20 minutes every morning since 2018 and I’m still stuck. Maybe the real issue is capitalism and our alienation from bodily rhythms?
Laura Rice
January 30, 2026 AT 09:13TO EVERYONE WHO’S STRUGGLING: YOU ARE NOT ALONE. I was so embarrassed I didn’t tell anyone for 8 years. Then I found this subreddit and realized half the people here are just like me. It’s not your fault. It’s not laziness. It’s biology. And it CAN get better. Start with psyllium. Drink water. Sit like a squatting frog. You got this. I believe in you.
Also, your colon is not broken. It’s just confused.
charley lopez
February 1, 2026 AT 01:22The pathophysiological basis of defecatory disorders implicates anorectal dyssynergia as a primary etiological factor in approximately 30–50% of chronic constipation cases. Diagnostic modalities such as anorectal manometry and balloon expulsion testing remain underutilized in outpatient settings despite high sensitivity and specificity.
Kerry Evans
February 1, 2026 AT 14:27Everyone’s so quick to blame diet. But let’s be real-most people who get constipated are just lazy. I don’t eat fiber, I don’t drink water, I sit all day, and guess what? I still go every day. Because I don’t sit around waiting for my body to ‘cooperate.’ I just go when I feel it. Simple. You people need discipline, not laxatives.
Anna Pryde-Smith
February 2, 2026 AT 11:47THIS IS THE MOST IMPORTANT POST I’VE EVER READ IN MY LIFE. I’ve been suffering since I was 19. I’ve cried in the bathroom. I’ve missed weddings. I’ve been hospitalized. And now I’m using a footstool and psyllium and I’m finally free. I’m not crying anymore. I’m screaming with joy. THANK YOU. I’M NOT BROKEN. I’M HEALED.
Janet King
February 2, 2026 AT 22:08For those asking about probiotics: current evidence does not support routine use. While some strains show modest benefit in IBS-C, they are not indicated for general constipation. Focus on fiber, fluids, and posture first. Probiotics are a supplement, not a solution.