When you hear Crohn’s disease and ulcerative colitis, it’s easy to think they’re the same thing. Both cause belly pain, diarrhea, and fatigue. Both are lifelong conditions. But they’re not the same - not even close. Knowing the difference isn’t just academic. It changes everything: how you’re diagnosed, what treatments work, and even what kind of surgery you might need.
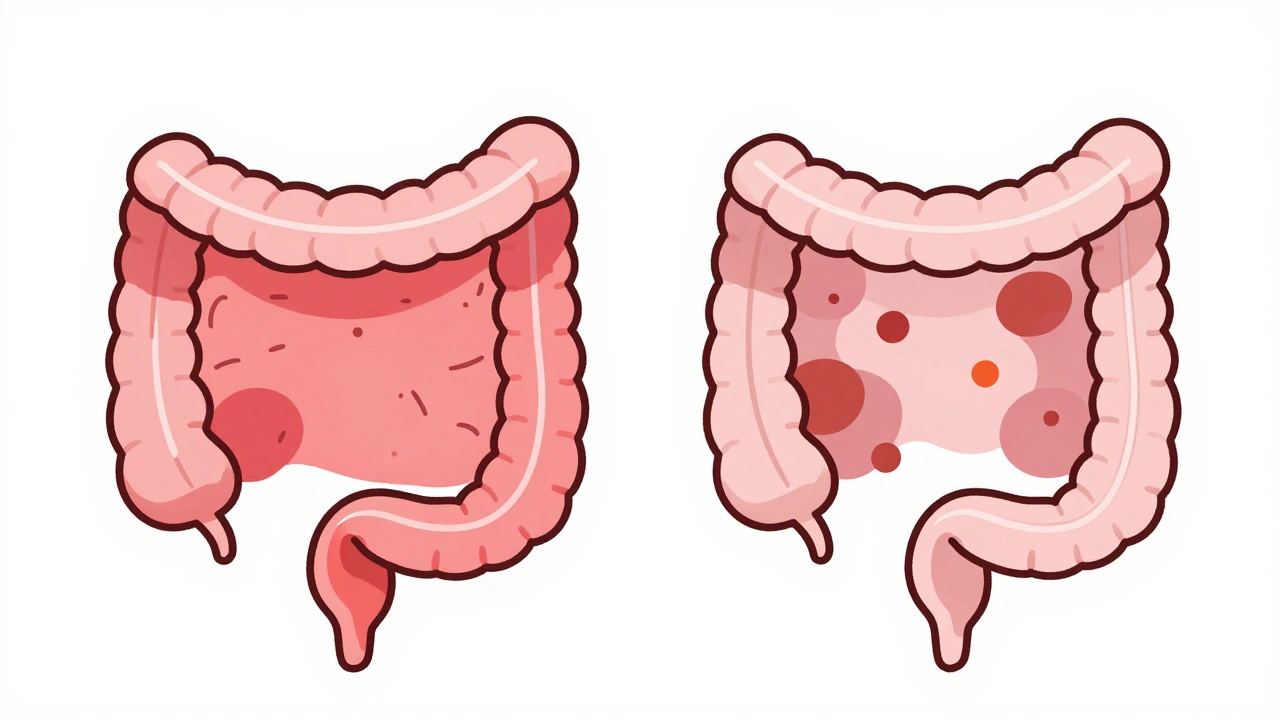
Where the Inflammation Happens
- Ulcerative colitis only affects the colon and rectum. It starts at the rectum and creeps upward in one continuous line. If you have it, your entire colon might be inflamed, or just the lower part. But it never jumps to the small intestine or stomach.
- Crohn’s disease can strike anywhere from your mouth to your anus. Most often, it hits the end of the small intestine (ileum) and the beginning of the colon. But it can also show up in your esophagus, stomach, or even around your anus. And here’s the kicker: it doesn’t go in a straight line. It skips. Healthy patches of tissue sit right next to inflamed ones - what doctors call "skip lesions."
This difference isn’t just about location. It’s about how deep the damage goes. Ulcerative colitis stays in the innermost layer of the bowel wall - the mucosa. Crohn’s disease punches all the way through - from the inside lining to the outer muscle and even the serosa. That’s why Crohn’s causes complications like fistulas and strictures that ulcerative colitis rarely does.
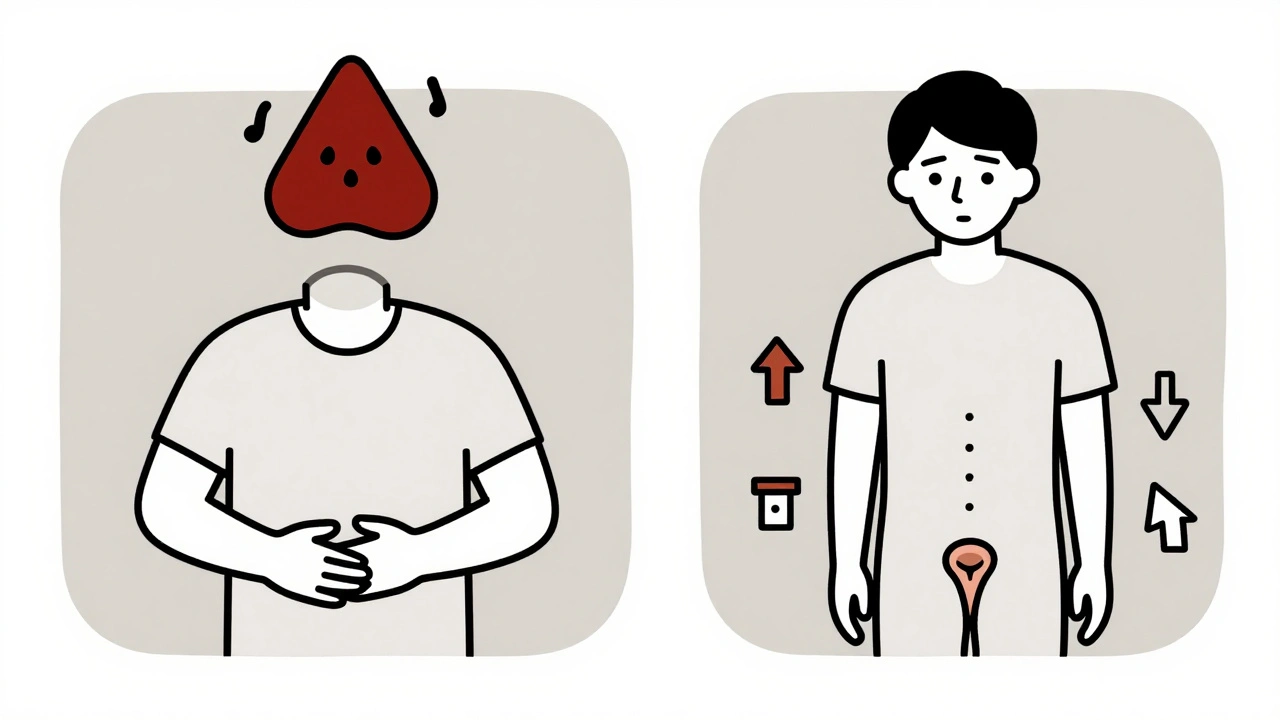
What Your Symptoms Look Like
Both conditions make you feel awful. But the details tell the story.
- If you have ulcerative colitis, you’re likely dealing with urgent, bloody diarrhea. Up to 75% of people report visible blood in their stool. The need to rush to the bathroom is constant. Fatigue and weight loss happen, but the biggest daily struggle is urgency and rectal bleeding.
- If you have Crohn’s disease, you might not bleed as much. Instead, you’re more likely to feel full quickly, lose weight because your body can’t absorb nutrients, or get abdominal pain from a narrowed intestine. Night sweats, mouth sores, and anal fistulas (painful tunnels between the bowel and skin) are far more common here.
And while both can cause joint pain, skin rashes, or eye inflammation, one condition has a unique liver link: primary sclerosing cholangitis (PSC). About 3 to 7% of people with ulcerative colitis develop this rare liver disease. Only about 1% of Crohn’s patients do.
How Doctors Tell Them Apart
No single blood test or scan can say for sure which one you have. Diagnosis is a puzzle. Doctors put together clues from:
- Colonoscopy: If the inflammation is continuous and starts at the rectum, it’s likely ulcerative colitis. If you see patchy damage, cobblestone-like tissue, or ulcers deep in the lining, it’s probably Crohn’s.
- Biopsies: Under the microscope, ulcerative colitis shows shallow inflammation. Crohn’s shows granulomas (tiny clusters of immune cells) in about 30% of cases - a big red flag.
- Imaging: MRI enterography or CT scans can show thickened bowel walls and fistulas - signs of Crohn’s. Capsule endoscopy (swallowing a tiny camera) finds small bowel damage in 70% of Crohn’s cases that colonoscopy misses.
- Blood and stool tests: pANCA antibodies show up in 60-70% of ulcerative colitis patients but only 10-15% of Crohn’s. Fecal calprotectin is high in both, but levels above 250 μg/g are more common in UC.
Even with all this, about 10-15% of cases are labeled "indeterminate colitis" at first. Doctors might need to watch for years before they’re sure. Some people initially diagnosed with ulcerative colitis later turn out to have Crohn’s - especially if they develop fistulas or need surgery.
Treatment: What Works for One Might Not Work for the Other
Some drugs help both, but others are chosen based on where the disease lives.
- Ulcerative colitis: Topical treatments like enemas or suppositories with 5-ASAs (mesalamine) work wonders for mild to moderate cases. They deliver medicine right to the inflamed colon. Remission rates hit 60-80%. If that fails, biologics like vedolizumab or ustekinumab are next. Surgery? It’s a cure. Removing the entire colon and rectum ends the disease for good.
- Crohn’s disease: Because it affects the whole gut, you need systemic drugs - pills or injections that work everywhere. Immunomodulators like azathioprine help about half of patients within a few months. Anti-TNF drugs like infliximab or adalimumab bring remission in 30-40% of cases. But here’s the catch: surgery doesn’t cure Crohn’s. You might have part of your intestine removed, but the disease almost always comes back nearby. Half of patients need another surgery within 10 years.
Emerging treatments show promise too. Fecal microbiota transplants (FMT) - essentially a poop transplant - led to remission in 32% of ulcerative colitis patients in a 2022 trial. For Crohn’s, the same treatment worked in only 22%. That’s a big gap. New drugs like mirikizumab (for Crohn’s) and etrolizumab (for UC) are in late-stage trials and could change the game soon.
Complications: The Real Difference
This is where the two diseases diverge most dramatically.
- Crohn’s disease: One in three people develop strictures (narrowed bowel sections) over time. One in four develops fistulas - abnormal tunnels connecting the bowel to the bladder, skin, or other organs. These can be painful, infected, and require surgery.
- Ulcerative colitis: The big danger is toxic megacolon - a rare but life-threatening swelling of the colon during a severe flare. It happens in about 5% of UC cases. Colon cancer risk also increases after 8-10 years of disease, so regular colonoscopies are critical.
Both can lead to malnutrition, but for different reasons. Crohn’s patients often can’t absorb vitamins and minerals because the small intestine is damaged. UC patients lose nutrients through constant diarrhea and bleeding.
Life With IBD: What Patients Say
Real people share their experiences on forums like Reddit’s r/IBD and the Crohn’s & Colitis Foundation’s community. Their stories highlight key patterns:
- Ulcerative colitis patients say stress is their biggest flare trigger - cited in 62% of posts.
- Crohn’s patients point to food: dairy (45%), high-fiber meals (38%), and spicy foods as common triggers.
- UC patients report rectal bleeding as their top concern. Crohn’s patients worry more about weight loss and nutrition.
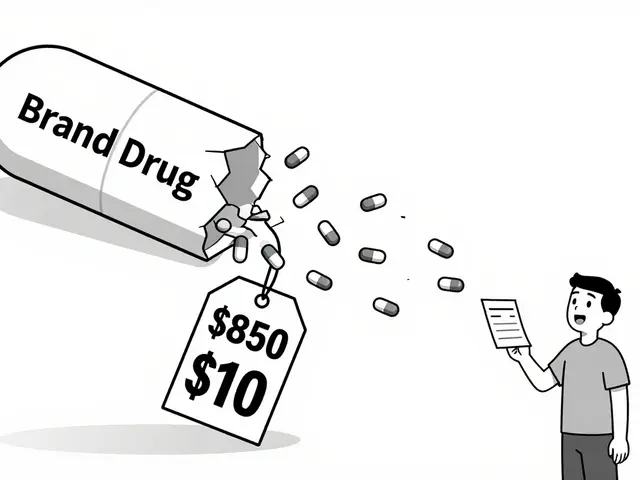
Costs are high for both. In the U.S., severe Crohn’s averages nearly $38,500 per year in medical expenses. Severe ulcerative colitis is close behind at $38,451. Mild cases cost less, but ongoing meds, doctor visits, and tests add up fast.
What You Need to Know
If you’ve been diagnosed with IBD, don’t just accept the label. Ask: Is this Crohn’s or ulcerative colitis? The answer changes your future. It tells you what to watch for, what treatments to try first, and whether surgery might one day be your best option.
And if you’re still unsure? You’re not alone. About 1 in 10 cases start as "indeterminate." That’s okay. Doctors will keep watching. Your body will keep talking. Sometimes, it takes years to hear the full story.
Either way, you’re not just managing a disease. You’re learning your body’s signals. And that knowledge - real, personal, specific - is your most powerful tool.
Can you have both Crohn’s disease and ulcerative colitis?
No, you can’t have both at the same time. They’re two distinct conditions. But about 10-15% of people are initially diagnosed with "indeterminate colitis" - meaning doctors can’t tell which one it is based on early tests. Over time, as symptoms or complications develop, the diagnosis usually becomes clearer. Some people originally thought to have ulcerative colitis turn out to have Crohn’s later, especially if they develop fistulas or skip lesions.
Is one condition worse than the other?
Neither is "worse" - they’re just different. Ulcerative colitis can be more urgent and bloody, with a higher risk of toxic megacolon. Crohn’s disease tends to cause more long-term complications like strictures and fistulas, and it can affect any part of the digestive tract. Surgery can cure ulcerative colitis, but it doesn’t cure Crohn’s. Which one is harder to live with depends on your symptoms, how you respond to treatment, and your personal tolerance for risk.
Can diet cure Crohn’s disease or ulcerative colitis?
No diet can cure either condition. But food choices can help manage symptoms. People with Crohn’s often find dairy, high-fiber foods, or spicy meals trigger flares. Those with ulcerative colitis may notice stress or certain sugars worsen diarrhea. Special diets like the low-FODMAP diet or specific carbohydrate diet can reduce discomfort, but they don’t stop the underlying inflammation. Medication is still needed to control the disease.
Do I need surgery if I have ulcerative colitis?
Surgery isn’t always needed, but it’s an option. About 10-15% of people with ulcerative colitis have their colon and rectum removed within 10 years - usually because medications aren’t working, cancer risk is high, or they’re having life-threatening complications. The surgery - called a total proctocolectomy with ileal pouch-anal anastomosis - removes the entire colon and rectum and creates a new internal pouch from the small intestine. After healing, most people can pass stool normally without a permanent bag.
Can Crohn’s disease turn into ulcerative colitis?
No, Crohn’s disease cannot turn into ulcerative colitis. They are separate diseases with different causes and patterns. But sometimes, the initial symptoms of Crohn’s - especially if it only affects the colon - can look a lot like ulcerative colitis. That’s why some people get misdiagnosed at first. Over time, if Crohn’s develops skip lesions, fistulas, or deep wall inflammation, the diagnosis is corrected.
Are there new treatments on the horizon?
Yes. For ulcerative colitis, drugs like etrolizumab and novel FMT approaches are showing strong results in trials. For Crohn’s, mirikizumab - a new biologic targeting interleukin-23 - has shown high remission rates in Phase 3 studies and could be approved soon. Researchers are also testing microbiome therapies, stem cell treatments, and personalized medicine based on genetic markers. These aren’t available yet, but they’re moving fast through clinical testing.




Francine Phillips
December 2, 2025 AT 16:22I just read this and felt like someone finally explained why my stomach hates me
no more guessing games with doctors
Katherine Gianelli
December 2, 2025 AT 22:44Wow this is so clear and kind
I’ve been struggling for years and this finally made sense
thank you for writing this like you actually care about people not just medical jargon
you made me feel seen
shalini vaishnav
December 4, 2025 AT 15:29This is basic gastroenterology 101 why are you treating it like groundbreaking science
in India we learn this in medical school before lunch
your entire article could’ve been a footnote
vinoth kumar
December 5, 2025 AT 20:57Man I’ve had Crohn’s for 12 years and this nailed it
especially the part about skip lesions and fistulas
I’ve had three surgeries and still no cure
but at least now I can explain it to my family without crying
bobby chandra
December 7, 2025 AT 15:38Let’s be real - the real difference isn’t in the colon or the ileum
it’s in how the medical system treats you
UC gets empathy because it bleeds
Crohn’s gets ignored because you just look ‘thin and tired’
and don’t get me started on how FMT trials are skewed
we need more equity in IBD research
not just more acronyms
Archie singh
December 8, 2025 AT 06:42Wow. Another feel-good article for the IBD influencers
did you forget to mention that 90% of these ‘new treatments’ are funded by pharma
and that ‘indeterminate colitis’ is just a fancy way of saying ‘we don’t know what we’re doing’
also PSC isn’t rare - it’s underdiagnosed because no one checks your liver
and yes, I’ve read the papers
you haven’t
Gene Linetsky
December 8, 2025 AT 12:58They’re hiding something
why is there no mention of glyphosate in the diet link?
why do all the studies ignore the microbiome collapse from Roundup
and why is the FDA still approving biologics when they’re just immunosuppressants in fancy bottles
the real cure is a 30-day raw food cleanse
but Big Pharma doesn’t want you to know that
ask yourself - who profits from lifelong meds?
Ignacio Pacheco
December 9, 2025 AT 21:55So let me get this straight - you’re telling me that if I stop eating kale, my Crohn’s might chill out?
but if I stop taking $12,000/month biologics, I die?
huh. That’s… oddly poetic
also, who wrote this? It’s weirdly accurate
and I’m suspicious
Jim Schultz
December 9, 2025 AT 22:40Actually, the most important thing you missed is that Crohn’s patients are statistically more likely to be diagnosed after a traumatic life event - divorce, death, job loss - and yet, no one ever asks about that in the clinic. We’re told to take pills, not talk. Meanwhile, UC patients get therapy referrals because ‘stress’ is ‘manageable.’ But if your gut is screaming because your dad died and you’re still paying for Humira? You’re just ‘non-compliant.’
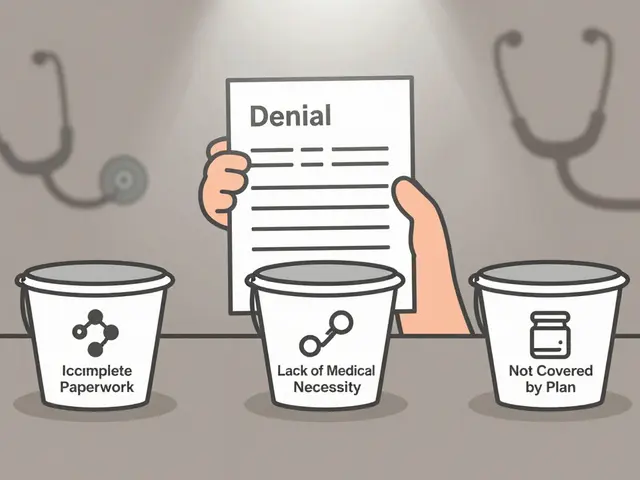
And don’t even get me started on how insurance denies FMT because it’s ‘experimental’ - while they approve $100K surgeries without blinking.
It’s not medicine. It’s a market.