Every year, thousands of patients in the U.S. receive the wrong medication-not because of a doctor’s mistake, but because two pills look too much alike on the shelf. One bottle says hydralazine, another says hydroxyzine. One label reads spironolactone, another spiramycin. To the untrained eye, they’re nearly identical. And in a busy pharmacy, with 50 prescriptions waiting and a ringing phone, it’s easy to grab the wrong one.
This isn’t a rare glitch. It’s a systemic problem. The Institute for Safe Medication Practices (ISMP) reports that nearly 1 in 5 medication errors involves look-alike or sound-alike (LASA) drugs. That’s not just a statistic-it’s a patient who gets the wrong heart drug, the wrong antibiotic, or worse. And the damage isn’t always reversible.
Why Look-Alike Packaging Is So Dangerous
It’s not just the names that fool you. It’s the packaging. Same font size. Same color scheme. Same shape bottle. Same cap. Two drugs, one look. A 2020 study from the University of Arizona found that when similar-looking medications are stored side by side, error rates jump by more than 60%. That’s because our brains don’t read every letter. We scan. We recognize patterns. And if two packages look the same, your brain assumes they are.
Take insulin. There are at least five types-Lantus, Humalog, NovoLog, Levemir, NPH. All white bottles. All with similar caps. One wrong syringe, one wrong dose, and a patient can slip into a coma. In one hospital, before they changed their storage layout, they had 3-4 insulin mix-ups every month. After separating them physically-putting each type in its own locked drawer with a bright label-they went 18 months with zero errors.
Physical Separation: The Simplest Fix
You don’t need fancy tech to stop this. You just need space-and discipline.
Start by mapping your pharmacy shelves. Group all high-risk LASA pairs together and then physically separate them. Put one drug on the top shelf, the other on the bottom. Use shelf dividers (cost: $200-$500 total). Put red tape on the shelf edge. Use different colored bins. Even a simple cardboard divider can make a difference.
For automated dispensing cabinets (ADCs), reconfigure drawers so that look-alike drugs can’t be side by side. If you have two drugs with similar names, don’t let them share the same row. Put one in drawer 3, the other in drawer 17. Make it impossible to grab both at once.
This method isn’t perfect. In high-volume pharmacies, space is tight. But even partial separation cuts errors by 30-62%, according to research. And it costs almost nothing compared to buying new software.

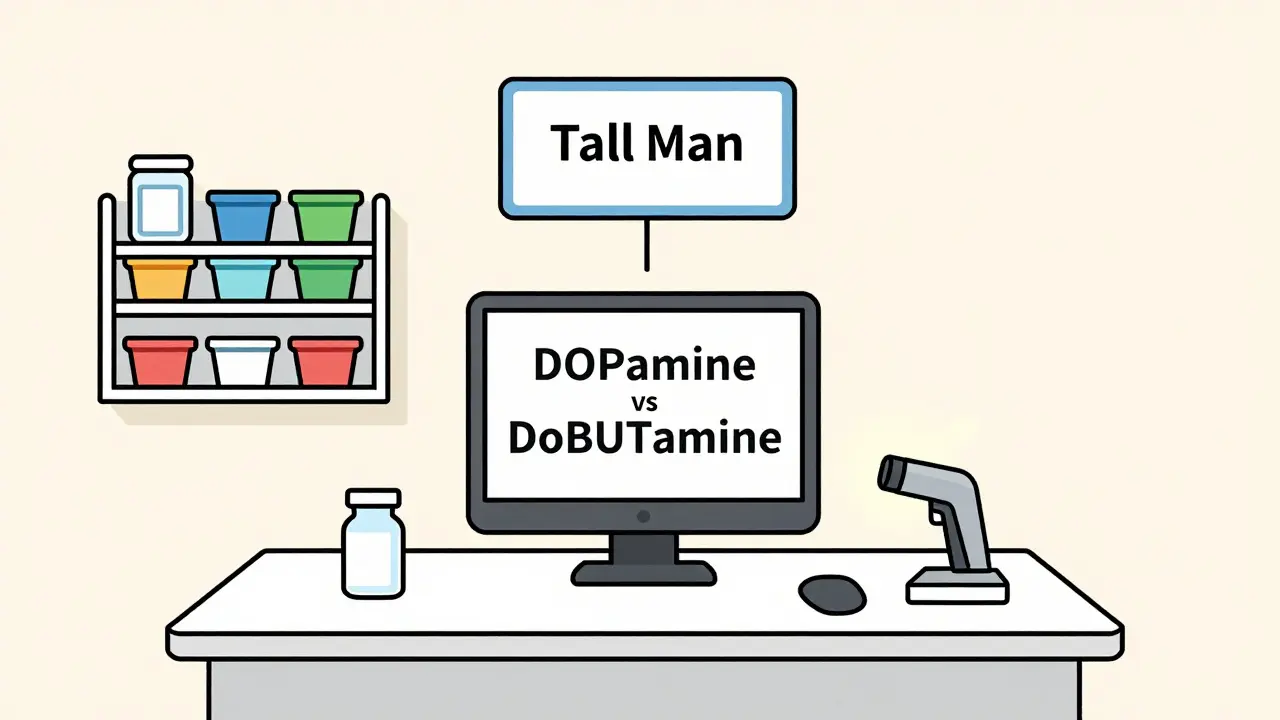
Tall Man Lettering: Making Differences Visible
When names are too close, change how they’re written.
Tall Man Lettering (TML) uses uppercase letters to highlight the parts of drug names that differ. For example:
- DOPamine vs. DoBUTamine
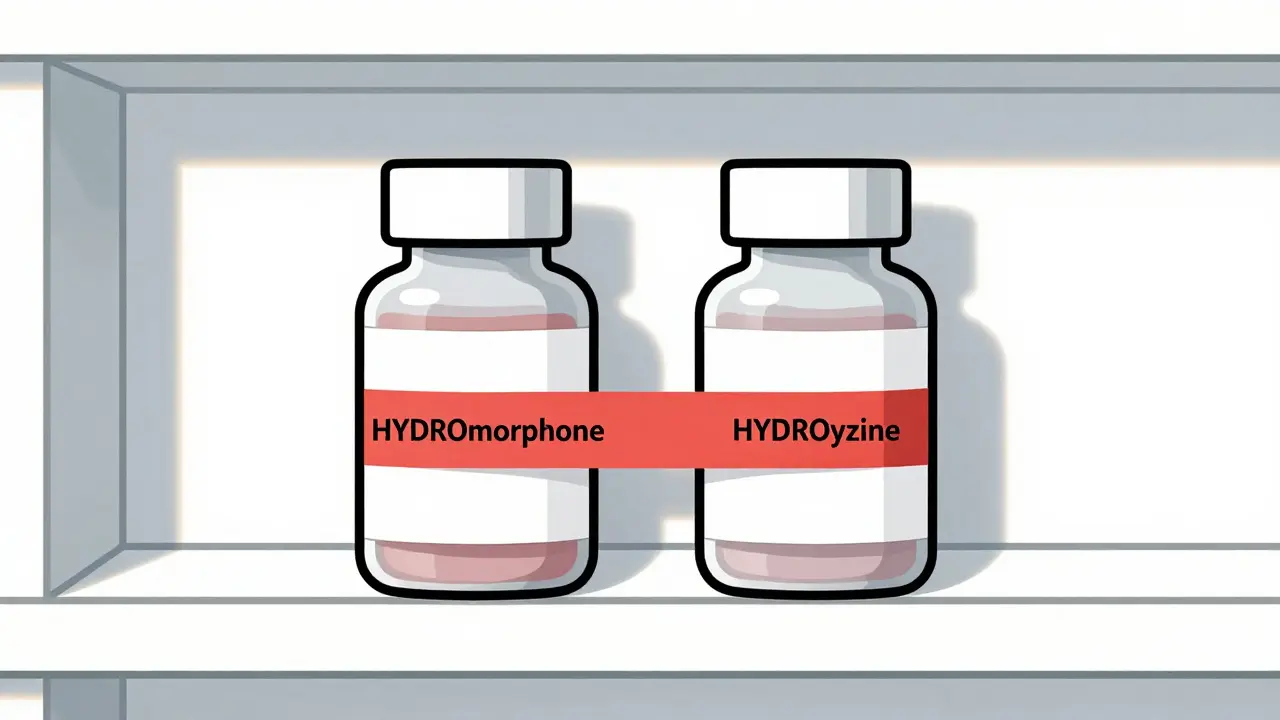
- HYDROmorphone vs. HYDROxyzine
- BUPRENORPHine vs. BUTORPHANol
It’s not magic-but it works. ISMP’s 2019 analysis showed a 47% drop in selection errors when TML was used consistently. The FDA recommends it for high-risk pairs. And since January 2024, the FDA has added 17 new drug pairs to its official list requiring TML.
But here’s the catch: not everyone uses it the same way. A 2022 survey found only 68% of hospitals use standardized TML formats. If your EHR system shows hydralazine in lowercase and another system shows HYDralazine, the warning is lost. That’s why you need to check your pharmacy software. Make sure your system displays TML the same way across all screens-prescribing, dispensing, and labeling.
Don’t rely on this alone. TML only fixes name confusion. It doesn’t help if two bottles look identical. As Dr. David Bates wrote in JAMA Internal Medicine, “Tall Man Lettering gives a false sense of security.” Use it-but pair it with something else.
Barcode Scanning: The Safety Net
Here’s the most powerful tool you have: barcode scanning.
When a pharmacist scans the medication and the patient’s wristband, the system checks: Is this the right drug? Right dose? Right patient? Right time? If not-it stops. No exceptions.
A 2021 AHRQ report found barcode scanning reduces medication administration errors by 86%. At Mayo Clinic, combining barcode scanning with physical separation eliminated 100% of potential errors in heparin and saline products over a year.
Yes, it costs money. $15,000 to $50,000 per pharmacy department. But consider this: one wrong dose of insulin can cost over $100,000 in emergency care and long-term treatment. Mayo Clinic’s program saved $287,000 a year-more than six times what it cost to install.
But here’s the problem: staff bypass it. They’re rushed. They think, “I know this one.” A 2021 study at UCSF found scanning failure rates of 5-12% because pharmacists skipped the scan. That’s why you need culture, not just tech. Train staff. Make scanning non-negotiable. Put reminders on screens. Reward compliance. Turn it into a habit.
How to Get Started: A 3-Step Plan
You don’t have to fix everything tomorrow. Start here:
- Run a LASA risk assessment. Use ISMP’s free Tool for Evaluating the Risk of Confusion Between Drug Names. It takes 8-12 hours for a typical pharmacy. Identify your top 10 most dangerous pairs. Common ones: metoprolol vs. methylprednisolone, clarithromycin vs. clonazepam, fentanyl vs. morphine.
- Implement physical separation. Rearrange your shelves. Use dividers. Put high-risk drugs far apart. Label everything clearly. Do this first-it’s low-cost and fast.
- Add TML and barcode scanning. Work with your EHR vendor to enable Tall Man Lettering. If you don’t have barcode scanning, prioritize it. Even a basic handheld scanner can cut errors in half.
Don’t wait for a mistake to happen. The Joint Commission requires pharmacies to address LASA risks. But compliance isn’t enough. You want to prevent harm-not just check a box.
What’s Next: The Future of Medication Safety
Technology is getting smarter. At Johns Hopkins, AI-powered systems are now scanning drug packaging images to spot visual similarities before they reach the shelf. These tools compare label layouts, font sizes, colors, and even cap shapes-flagging potential look-alikes before they’re even stocked.
By late 2025, the National Council for Prescription Drug Programs (NCPDP) will launch a standardized LASA data format. That means every pharmacy system will talk the same language. No more mismatched TML. No more confusion between systems.
But the real change won’t come from tech alone. It’ll come from culture. From pharmacists who double-check. From technicians who speak up. From managers who make safety a priority-not an afterthought.
Medication safety isn’t about perfection. It’s about layers. Physical separation. Clear labeling. Scanning. Training. Culture. When you stack them together, you don’t just reduce errors-you prevent tragedies.
One pharmacy in Brisbane started with just shelf dividers and TML. In six months, their wrong-medication reports dropped by 70%. No new software. No big budget. Just attention to detail.
That’s the power of small changes. And it’s within your reach.






Stephen Craig
January 5, 2026 AT 05:26It’s not about the tech. It’s about slowing down long enough to see the difference between HYSO and HYDRO. We’ve all been rushed. But one second of hesitation saves a life.
Jack Wernet
January 6, 2026 AT 11:04The systemic nature of this issue cannot be overstated. The convergence of cognitive bias, environmental design, and institutional inertia creates a perfect storm for error. While technological interventions such as barcode scanning and Tall Man Lettering are indispensable, they remain secondary to the cultivation of a safety-first culture within pharmacy practice.
Charlotte N
January 7, 2026 AT 08:23I’ve seen this happen… the bottles look the same… the names are so close… and you’re tired… and the line is long… and you just grab… and then you realize… oh god… why didn’t someone put a red dot on one… why didn’t we just… separate them…
Uzoamaka Nwankpa
January 7, 2026 AT 17:23This is why I don’t trust pharmacies anymore. No one cares until someone dies. And even then, they just update the policy and move on.
Chris Cantey
January 9, 2026 AT 07:09The real problem isn’t the packaging. It’s that we’ve outsourced critical thinking to labels and scanners. We’ve turned pharmacists into order-takers. And when you stop thinking, you stop seeing. The machine doesn’t care if hydralazine looks like hydroxyzine. Only you do.
Abhishek Mondal
January 11, 2026 AT 05:19Let’s be honest: most of these so-called ‘solutions’ are band-aids on a bullet wound. The real issue is that pharmaceutical companies design packaging to be visually indistinguishable to maximize shelf space and minimize cost. This isn’t negligence-it’s corporate malice. And until we hold manufacturers legally liable for look-alike designs, we’re just rearranging deck chairs on the Titanic.
en Max
January 11, 2026 AT 14:43While the implementation of physical separation protocols and Tall Man Lettering is empirically validated, the efficacy of these measures is contingent upon consistent operational adherence. Furthermore, the integration of barcode scanning necessitates not only infrastructural investment but also the institutionalization of behavioral compliance through reinforcement-based training paradigms. The data from Mayo Clinic, while compelling, must be contextualized within the broader framework of human factors engineering.
Angie Rehe
January 13, 2026 AT 01:50Oh please. You think putting tape on shelves fixes anything? Half the pharmacists I work with don’t even read the labels. They just scan and walk away. This isn’t a design problem-it’s a people problem. And nobody wants to fix people.
josh plum
January 14, 2026 AT 22:13They’re hiding this on purpose. Big Pharma doesn’t want you to notice how similar these drugs look. They want you to make mistakes so they can sell you more meds later. Wake up. This is a profit play.
John Ross
January 15, 2026 AT 00:07Physical separation is the lowest-hanging fruit. Why aren’t we doing this everywhere? The cost-benefit ratio is absurdly favorable. If we can reduce errors by 60% with $500 in dividers, why are we still spending millions on software that doesn’t change human behavior?
Ashley Viñas
January 16, 2026 AT 02:13It’s funny how everyone talks about tech fixes but ignores the real culprit: the pharmacy tech who’s been working 12 hours straight and just wants to go home. No amount of TML will fix exhaustion. We need staffing reform-not just shelf rearrangement.
Brendan F. Cochran
January 17, 2026 AT 02:30why do we even have so many drugs that sound the same? someone should just rename them all. like call hydralazine ‘heartzap’ and hydroxyzine ‘itchnix’. problem solved. dumb.
Michael Rudge
January 18, 2026 AT 17:55Oh wow. A whole essay on how to not grab the wrong pill. And yet, here we are, still doing it. Brilliant. Let’s all take a moment to applaud the genius who realized that putting things far apart might help. Truly groundbreaking.